Abstract
Urostomy formation represents a significant surgical intervention employed in the management of various bladder dysfunctions, ranging from malignancy to neurogenic bladder and, increasingly, complications arising from substance abuse, notably ketamine-induced cystitis. This report provides a comprehensive overview of urostomy surgery, covering various surgical techniques, long-term functional outcomes, potential complications, psychosocial impacts on patients, and the resources available to support individuals adapting to life with a urostomy. Special attention is given to the unique challenges presented by urostomy management in patients with histories of substance abuse, including adherence to care regimens and psychological comorbidities. Furthermore, we explore the factors influencing the average duration of urostomy use and discuss potential advancements in surgical techniques and management strategies aimed at improving patient outcomes and quality of life.
Many thanks to our sponsor Maggie who helped us prepare this research report.
1. Introduction
The urinary bladder plays a crucial role in the storage and regulated expulsion of urine. When bladder function is compromised due to disease, trauma, or congenital abnormalities, urinary diversion procedures become necessary to ensure effective drainage of urine. Among these procedures, urostomy formation is a commonly performed surgical option, involving the creation of an external stoma through which urine is diverted from the ureters. The necessity of urostomy formation can arise from several etiologies including bladder cancer, spinal cord injury, and interstitial cystitis. Recent evidence has highlighted ketamine abuse as a growing cause of severe bladder damage necessitating urostomy (Shahani et al., 2007). Chronic ketamine abuse can cause ketamine-induced ulcerative cystitis (KIUC). The resulting chronic inflammation and fibrosis of the bladder often lead to reduced bladder capacity, severe pain, and urinary incontinence and, in severe cases, the definitive solution is cystectomy with subsequent urinary diversion (Thurtle et al., 2014). This report aims to provide a comprehensive overview of urostomy management, from surgical techniques to long-term considerations, with particular emphasis on the psychosocial impact and specific challenges presented by individuals requiring urostomies due to ketamine-induced bladder dysfunction.
Many thanks to our sponsor Maggie who helped us prepare this research report.
2. Surgical Techniques for Urostomy Formation
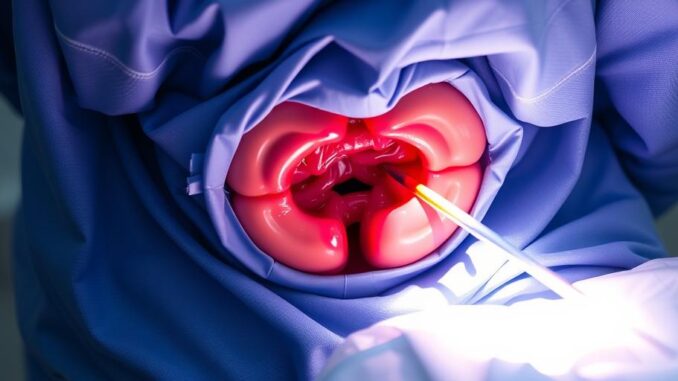
Urostomy formation involves the surgical construction of a stoma, an opening on the abdominal wall, to which the ureters are connected, allowing urine to be collected in an external pouch. Several surgical techniques exist, each with its advantages and disadvantages:
-
Ileal Conduit: This is the most common type of urostomy. A segment of the ileum (small intestine) is isolated and anastomosed to the ureters. One end of the ileal segment is brought out through the abdominal wall to create the stoma. The ileal conduit provides a reliable conduit for urine flow, but it also involves bowel resection, which can lead to complications such as bowel obstruction, electrolyte imbalances, and malabsorption in rare cases (Dhar et al., 2016).
-
Cutaneous Ureterostomy: This simpler technique involves directly attaching the ureters to the skin. It avoids bowel resection but often results in poorly formed stomas, increasing the risk of stenosis, leakage, and skin irritation. This technique is typically reserved for patients with limited life expectancy or significant comorbidities that preclude more complex procedures (Musleh et al., 2015).
-
Transureteroureterostomy (TUU) with Ureterostomy: This method involves connecting one ureter to the contralateral ureter, which is then brought to the skin as a stoma. While avoiding bowel resection, TUU poses the risk of compromising the healthy ureter if complications arise. It is rarely performed in the context of radical cystectomy but may be considered in select cases of unilateral ureteral obstruction.
-
Continent Cutaneous Urostomy: These techniques, such as the Indiana pouch or Mainz pouch, involve creating an internal pouch from bowel segments that can store urine. The patient catheterizes the pouch through a stoma several times a day to empty it. These continent diversions offer greater patient autonomy and eliminate the need for an external pouch, but they require significant patient compliance and are associated with higher complication rates, including pouch stones, infections, and difficulty catheterizing (Hautmann et al., 2003).
The choice of surgical technique depends on various factors, including the patient’s overall health, the underlying cause of bladder dysfunction, surgeon experience, and patient preference. In patients with ketamine-induced cystitis, the severity of bladder damage and the presence of other comorbidities may influence the selection of the optimal surgical approach. The ileal conduit remains the most frequently utilized procedure, because of its robustness and familiarity among surgeons. However, in appropriately selected patients, continent cutaneous urostomies can provide a significant improvement in quality of life.
Many thanks to our sponsor Maggie who helped us prepare this research report.
3. Post-Operative Care and Daily Life Adjustments
Following urostomy surgery, patients require comprehensive post-operative care to ensure proper healing and adaptation to life with a stoma. This includes:
-
Stoma Care: Patients and caregivers are educated on proper stoma care techniques, including cleaning the stoma and surrounding skin, changing the pouching system, and recognizing signs of complications such as skin irritation, infection, or stoma retraction. The selection of appropriate pouching systems and accessories is critical for maintaining skin integrity and preventing leakage. Ideally, the pouch should be lightweight, skin-friendly, and secure (Burch, 2007).
-
Dietary Modifications: Certain dietary adjustments may be recommended to minimize urine odor, reduce the risk of urinary tract infections (UTIs), and prevent dehydration. Adequate fluid intake is crucial for maintaining urine output and preventing urinary stasis. Foods and beverages known to cause urinary odor, such as asparagus, garlic, and alcohol, may be restricted. Cranberry juice or supplements may be recommended to prevent UTIs, although evidence supporting their efficacy is limited (Hisano et al., 2012).
-
Activity and Exercise: Most patients can resume their usual activities and exercise routines after urostomy surgery, but certain precautions may be necessary. Heavy lifting and strenuous activities may need to be avoided during the initial recovery period to prevent strain on the abdominal muscles and stoma site. A stoma guard may be recommended for contact sports or activities that pose a risk of injury to the stoma.
-
Emotional and Psychological Support: Adjusting to life with a urostomy can be emotionally challenging. Patients may experience anxiety, depression, body image concerns, and social isolation. Counseling, support groups, and peer support can provide valuable emotional support and coping strategies. Addressing psychological distress and promoting positive body image are essential components of comprehensive urostomy care.
Many thanks to our sponsor Maggie who helped us prepare this research report.
4. Potential Complications of Urostomy Formation
Urostomy surgery is associated with a range of potential complications, which can be broadly classified as early or late complications:
-
Early Complications: These occur within the first few weeks or months after surgery and include wound infection, bleeding, urinary leakage, stoma necrosis, and bowel obstruction. Prompt recognition and management of these complications are essential to prevent further morbidity. Surgical revision may be necessary in some cases.
-
Late Complications: These develop months or years after surgery and include stomal stenosis, parastomal hernia, ureteroenteric stricture, hydronephrosis, pouch stones (in continent diversions), and metabolic abnormalities (e.g., hyperchloremic metabolic acidosis with ileal conduits). Regular follow-up and surveillance are crucial for detecting and managing late complications. Ureteroscopic dilation, percutaneous nephrostomy, or surgical revision may be required to address these issues (Hussein et al., 2014).
-
Specific Considerations in Ketamine-Induced Cystitis: Patients with ketamine-induced cystitis may be at increased risk of certain complications, such as stomal stenosis and ureteroenteric stricture, due to the chronic inflammation and fibrosis associated with the condition. Furthermore, their history of substance abuse may complicate post-operative pain management and adherence to follow-up appointments. A multidisciplinary approach involving urologists, pain management specialists, and addiction counselors is essential for optimizing outcomes in this patient population.
Many thanks to our sponsor Maggie who helped us prepare this research report.
5. Psychological and Social Impact
The psychological and social impact of urostomy formation can be profound, affecting various aspects of a patient’s life:
-
Body Image and Self-Esteem: The presence of a stoma and pouch can significantly alter body image and self-esteem, leading to feelings of shame, embarrassment, and decreased sexual function. Patients may avoid social situations and intimacy due to concerns about leakage, odor, or negative reactions from others. Counseling and support groups can help patients develop coping strategies and improve body image.
-
Social Isolation: The fear of leakage or odor can lead to social isolation and withdrawal from activities that were previously enjoyed. Patients may feel self-conscious about their stoma and avoid situations where they might feel exposed or vulnerable. Encouraging patients to participate in support groups and social activities can help combat social isolation.
-
Anxiety and Depression: Urostomy formation can trigger anxiety and depression, particularly in individuals with pre-existing mental health conditions. The challenges of managing a stoma, the fear of complications, and the impact on body image can contribute to these mental health issues. Cognitive behavioral therapy (CBT) and medication may be helpful in managing anxiety and depression.
-
Sexual Function: Urostomy surgery can affect sexual function, both physically and psychologically. Nerve damage during surgery can lead to erectile dysfunction in men, while changes in body image and self-esteem can affect sexual desire and arousal in both men and women. Counseling, medication, and supportive devices can help address these issues (Frey et al., 2012).
-
Specific Challenges in Ketamine Abuse: Patients with a history of ketamine abuse may experience unique psychological challenges related to urostomy formation. Guilt, shame, and remorse about their past substance abuse may exacerbate their emotional distress. Additionally, their history of addiction may complicate their ability to cope with the physical and emotional demands of urostomy management. Addiction counseling and relapse prevention strategies may be necessary to support these patients.
Many thanks to our sponsor Maggie who helped us prepare this research report.
6. Support Resources and Rehabilitation
Various support resources and rehabilitation programs are available to assist patients in adapting to life with a urostomy:
-
Wound, Ostomy, and Continence Nurses (WOCNs): WOCNs are specialized nurses who provide expert care and education to patients with ostomies, wounds, and continence issues. They can provide guidance on stoma care, pouching systems, skin care, and management of complications. WOCNs also offer emotional support and counseling.
-
Support Groups: Support groups provide a safe and supportive environment for patients to share their experiences, learn from others, and receive encouragement. These groups can be invaluable in helping patients cope with the emotional challenges of urostomy formation.
-
Online Resources: Numerous online resources, including websites, forums, and social media groups, offer information and support to patients with urostomies. These resources can provide access to educational materials, patient testimonials, and opportunities to connect with others who have similar experiences.
-
Rehabilitation Programs: Comprehensive rehabilitation programs may include physical therapy, occupational therapy, and psychological counseling to help patients regain their physical function, improve their coping skills, and enhance their quality of life. These programs can be tailored to meet the individual needs of each patient.
-
Specific Resources for Ketamine Abuse: Patients with ketamine-induced bladder dysfunction may benefit from specialized addiction treatment programs and support groups. These programs can help them address their substance abuse issues, develop coping strategies for managing cravings, and prevent relapse. Integrating addiction treatment with urological care is essential for optimizing outcomes in this patient population.
Many thanks to our sponsor Maggie who helped us prepare this research report.
7. Average Time of Urostomy Use and Factors Influencing Duration
The average duration of urostomy use varies significantly depending on the underlying cause of bladder dysfunction, patient characteristics, and the presence of complications. In some cases, urostomy formation is a temporary measure intended to allow for bladder healing or recovery from surgery. In other cases, it is a permanent solution for irreversible bladder damage or dysfunction.
-
Temporary Urostomies: These are typically used for a period of weeks or months to allow for bladder healing after surgery or trauma. Once bladder function has recovered, the urostomy can be reversed. The duration of temporary urostomy use depends on the rate of healing and the absence of complications.
-
Permanent Urostomies: These are intended to provide long-term urinary diversion for patients with irreversible bladder damage or dysfunction. The duration of permanent urostomy use can range from several years to the remainder of the patient’s life. Factors influencing the duration of permanent urostomy use include the patient’s overall health, the presence of complications, and the patient’s adherence to care regimens.
-
Specific Considerations in Ketamine Abuse: In patients with ketamine-induced cystitis, urostomy formation is often a permanent solution for severe bladder damage. The average duration of urostomy use in this population is likely to be long-term, as the bladder damage is typically irreversible. However, successful management of the underlying addiction and prevention of further ketamine use are crucial for optimizing long-term outcomes and preventing complications. The duration of urostomy can be shortened only via reconstructive surgery, which is an invasive procedure.
Factors influencing the duration of urostomy use include:
- Underlying cause of bladder dysfunction: The severity and reversibility of the underlying condition can affect the duration of urostomy use.
- Patient characteristics: Age, overall health, and adherence to care regimens can influence the duration of urostomy use.
- Presence of complications: Complications such as stomal stenosis, ureteroenteric stricture, and parastomal hernia can necessitate surgical revision or other interventions, potentially prolonging or shortening the duration of urostomy use.
- Surgical technique: The type of urostomy performed (e.g., ileal conduit, cutaneous ureterostomy, continent cutaneous urostomy) can affect the risk of complications and the long-term maintenance requirements.
Many thanks to our sponsor Maggie who helped us prepare this research report.
8. Future Directions and Advancements
Several advancements in surgical techniques and management strategies are being explored to improve outcomes and quality of life for patients with urostomies:
-
Robotic-Assisted Surgery: Robotic-assisted surgery offers the potential for more precise and less invasive urostomy formation. Studies have shown that robotic-assisted radical cystectomy with ileal conduit diversion can result in shorter hospital stays, reduced blood loss, and fewer complications compared to open surgery (Khan et al., 2010).
-
Minimally Invasive Techniques: Laparoscopic and percutaneous techniques are being developed to address complications such as stomal stenosis and ureteroenteric stricture. These techniques can reduce the need for open surgical revision and minimize patient morbidity.
-
Tissue Engineering: Researchers are exploring the use of tissue engineering to create functional bladder substitutes that can be implanted in patients with bladder dysfunction. This approach could potentially eliminate the need for urinary diversion and restore normal bladder function.
-
Personalized Medicine: Advances in genomics and proteomics are paving the way for personalized approaches to urostomy management. By identifying individual risk factors and tailoring treatment strategies accordingly, it may be possible to improve outcomes and reduce complications.
-
Enhanced Psychological Support: Developing more effective psychological interventions, such as mindfulness-based therapies and peer support programs, can help patients cope with the emotional challenges of urostomy formation and improve their quality of life.
Further research is needed to evaluate the long-term efficacy and cost-effectiveness of these advancements. Continued collaboration between urologists, nurses, psychologists, and other healthcare professionals is essential for optimizing the care of patients with urostomies.
Many thanks to our sponsor Maggie who helped us prepare this research report.
9. Conclusion
Urostomy formation remains a critical surgical option for managing various bladder dysfunctions. While effective in diverting urine, it presents significant challenges for patients, encompassing surgical complications, daily life adjustments, and psychosocial impacts. Managing urostomies, especially in the context of ketamine-induced cystitis, demands a holistic, multidisciplinary approach. This encompasses meticulous surgical technique, comprehensive post-operative care, robust psychological support, and targeted interventions to address addiction-related challenges. Future research focusing on minimally invasive techniques, personalized medicine, and enhanced psychological support holds the promise of improving outcomes and quality of life for individuals living with urostomies. By addressing the unique needs of this patient population, healthcare providers can empower them to lead fulfilling and productive lives.
Many thanks to our sponsor Maggie who helped us prepare this research report.
References
Burch, J. (2007). Preoperative stoma site marking: a systematic review. Journal of Wound, Ostomy and Continence Nursing, 34(6), 595-599.
Dhar, V. K., Bhandari, M., & Kapoor, R. (2016). Intestinal complications after radical cystectomy and urinary diversion: a systematic review. Urology, 87, 1-7.
Frey, A., Hürlimann, S., Eberli, D., & Kessler, T. M. (2012). Body image and sexuality in patients with urinary stomas: a systematic review. Journal of Wound, Ostomy and Continence Nursing, 39(6), 587-593.
Hautmann, R. E., Abol-Enein, H., Davidsson, T., Koch, T. W., Lin, A. T., Mansson, W., … & Studer, U. E. (2003). Urinary diversion: current status and future perspectives. Urology, 62(4), 7-17.
Hisano, M., Terawaki, H., & Yamamoto, H. (2012). Cranberries and lower urinary tract infection prevention. Clinics (Sao Paulo), 67(6), 661-668.
Hussein, A. A., El-Maadawy, M., El-Kappany, H. A., Nabeeh, A., & Mokhtar, A. A. (2014). Long-term complications after radical cystectomy and urinary diversion: a single-center experience. World Journal of Urology, 32(6), 1505-1510.
Khan, M. S., Gan, C., Ahmed, K., Ismail, A., Shamim Khan, M., & Dasgupta, P. (2010). Robotic versus open radical cystectomy: systematic review and meta-analysis. European Urology, 57(5), 819-829.
Musleh, M. A., Kim, D. H., & Kuo, P. C. (2015). Cutaneous ureterostomy: revisited. The American Surgeon, 81(1), 75-78.
Shahani, R., Kwong, A., Paraiso, M. F., & Stoller, M. L. (2007). Lower urinary tract symptoms associated with ketamine abuse. Urology, 69(5), 810-812.
Thurtle, D. R., Lawrenson, A. L., & Shahani, R. (2014). Ketamine-induced uropathy: a contemporary review. World Journal of Urology, 32(2), 341-348.


Be the first to comment