Summary
This article offers a comprehensive guide to opioid addiction recovery, summarizing key steps and insights from leading research in 2024. It emphasizes the importance of medication-assisted treatment, behavioral therapy, and strong support systems. The article offers practical and actionable advice for individuals navigating the path to recovery.
** Main Story**
Okay, so tackling opioid addiction is tough, no doubt. But, it’s absolutely doable. Recent research – think 2024 stuff – really shines a light on what works when guiding people towards lasting recovery. It’s not a one-size-fits-all thing, but here’s a breakdown based on what’s current:
The First Hurdle: Acknowledgment
First, you gotta get real. Opioid addiction? It’s a chronic disease, and it relapses. It is not some kind of personal failing, okay? And accepting that, really internalizing it, that’s your starting point. It’s the key to reaching out for help. You know, I saw a stat recently highlighting how crushing stigma can be. It’s a huge barrier to recovery, so we need supportive environments, desperately. Without them, what chance do people have?
Seek Professional Guidance
Next up, get a doctor involved. It’s crucial to explore treatment options tailored to your situation. The evidence points strongly towards medication-assisted treatment (MAT) alongside behavioral therapies. You often get the best results using them together, you know. MAT, in essence, helps reset your brain chemistry, cuts down on cravings, and nips those nasty withdrawal symptoms in the bud.
Diving Deeper into Medication-Assisted Treatment (MAT)
Now, let’s unpack MAT a little. We’re talking medications like buprenorphine, methadone, or naltrexone – but it’s not just about popping pills. It needs counseling and support to really work. A common misconception? That it’s just swapping one drug for another. Not true. What it actually does is manage the addiction. This frees you up to focus on those crucial lifestyle changes that make or break recovery. Ultimately, which medication you use is a deeply personal medical call. Sit down with your doctor, have that discussion.
Embrace the Power of Therapy
Then there’s behavioral therapy. This is where you start reshaping those attitudes and behaviors fueling the addiction. Cognitive-behavioral therapy, or CBT, is fantastic. It equips you with the tools to spot, dodge, and handle those high-risk situations that can trigger a relapse. And there’s more to it than just CBT. Contingency management, for example, uses positive reinforcement. Who doesn’t respond to a little reward for good behavior?
Build Your Tribe: Support is Key
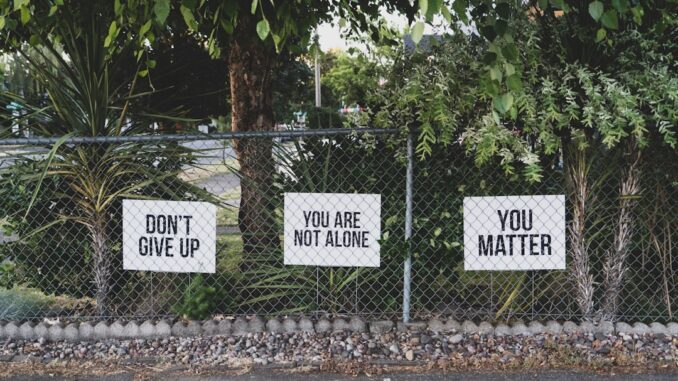
Let me be blunt. Going it alone? Recovery’s gonna be ten times harder. Reach out. Find those close friends, family, support groups – or even sober social networks. These connections? They’re your lifeline, offering encouragement, guidance, and that safe space where you can just… share. If addiction’s strained relationships, don’t give up on family therapy. It can really work wonders for rebuilding trust and communication.
Coping Strategies: Your New Toolkit
Let’s face it, addiction often grows from using drugs to self-medicate. To numb stress, trauma, or tackle underlying mental health issues. Long-term recovery means learning new, healthy coping strategies. It might be exercise, mindfulness, relaxation techniques, or simply rediscovering hobbies you love. I remember reading about one study that showed a direct correlation between the number of hobbies a person engaged in and their success in recovery. Interesting, right?
Taming the Triggers
Triggers are sneaky. They’re those people, places, things, or even moods that remind you of using and set off cravings. You gotta identify yours, specifically. Then, arm yourself with strategies to avoid them or, if that’s impossible, cope with them effectively. Changing routines, sidestepping certain environments, mastering mindfulness… it all helps.
Riding Out the Cravings
Cravings are inevitable; they’re part of the process. Don’t beat yourself up about it! Instead, prepare for them. Have your go-to strategies ready. Talk to your therapist, reach out to your support network, dive into a distracting activity, practice mindfulness, or just remind yourself why you’re doing this.
A Life Worth Living, Drug-Free
Remember, recovery isn’t just about not using. It’s about building a life you actually want to live, a life you’re excited about. So chase new interests, set those big, meaningful goals, throw yourself into activities you enjoy, and, crucially, prioritize your own personal growth.
Relapse Happens. Don’t Panic.
Okay, last thing, and this is important. Relapse is a possibility. It happens. Don’t let it derail you. It’s not a sign of failure, just a bump in the road. Treat it as a learning experience. Figure out what led to it, tweak your recovery plan, and recommit to your sobriety. I’ve seen so many people who stumbled but got back up, stronger than before. You can too.
Some 2024 research also highlighted some interesting points:
- The rise of new psychoactive substances, like xylazine (often mixed with fentanyl), poses new threats to public health. It’s a scary world out there, so keep informed.
- Ketamine use disorder is emerging as a concern. It needs more investigation, and we need to develop targeted interventions.
- On a brighter note, most teenagers are reporting less use of alcohol, tobacco, cannabis, and vaping. That’s an unprecedented trend! Good news for the next generation.
- New research explores the role of myelination (a brain process linked to learning) in the development of opioid addiction. The more we understand the science, the better we can fight this thing.
So there you have it. Stick to these steps, stay informed, and remember, you’re not alone in this. Recovery is a challenge, but it’s absolutely within reach. And believe me, a healthier, more fulfilling future is waiting for you on the other side.


Be the first to comment