Navigating the Road to Recovery: A Comprehensive Guide to Overcoming Opioid Use Disorder
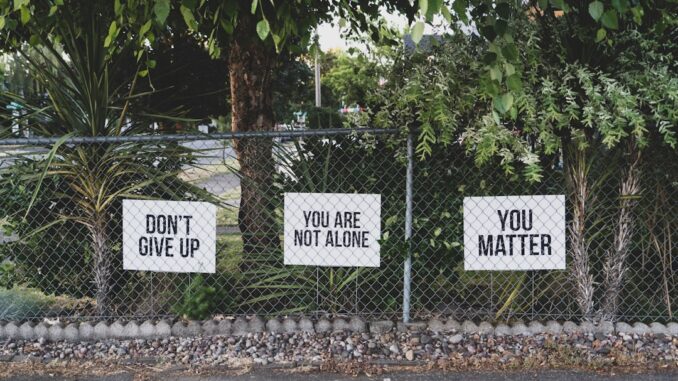
Embarking on the path to recovery from opioid addiction is, without a doubt, one of the most courageous decisions a person can ever make. It’s not just a declaration; it’s a profound commitment to reclaim your life from the grip of a powerful adversary. Opioid Use Disorder (OUD) isn’t just a challenge for a few; it affects millions globally, quietly, insidiously, often tearing at the fabric of lives and communities. But here’s the thing, despite how overwhelming it might feel right now, recovery isn’t just a hopeful whisper; it’s a tangible, achievable reality when you approach it with the right tools, the right support, and an unwavering resolve.
This isn’t about shaming or judgment. Instead, consider this a practical, empathetic guide, one designed to light the way forward, offering concrete steps and insights drawn from both professional understanding and the shared experiences of those who’ve walked this path before. You’re definitely not alone in this journey.
Unpacking Opioid Withdrawal: The Body’s Symphony of Absence
When you make the decision to stop using opioids, your body, which has grown accustomed to their presence, reacts rather dramatically to their sudden absence. This reaction is what we call withdrawal, and it’s often the first, and certainly one of the most daunting, hurdles in the recovery process. The symptoms can span a wide spectrum, from what feels like a minor discomfort to an almost unbearable distress that can make every fiber of your being scream for relief.
Think of it this way: your brain has adjusted its chemistry to the constant influx of opioids, relying on them to regulate pain, pleasure, and even basic bodily functions. When that external supply is cut off, your body goes into overdrive, trying to re-establish its natural balance, and that internal struggle manifests in a host of uncomfortable symptoms. Common initial symptoms include nausea, vomiting, relentless muscle aches that feel like deep bone pain, restless legs that simply won’t stay still, profound anxiety that can feel like a tightening vice around your chest, and an insomnia so severe you might feel you’re going mad from lack of sleep.
I remember my friend, Sarah, describing her early withdrawal phase. She said it was like ‘the worst flu you’ve ever had, amplified by a thousand’. She talked about relentless chills that left her shivering uncontrollably, even under a pile of blankets, followed by waves of hot flashes and drenching sweats. The body aches, she said, were so intense they made it almost impossible to find a comfortable position, let alone get out of bed. Then there were the goosebumps, the diarrhea, the constant yawning, and pupils dilated so wide she felt like her eyes were absorbing all the light in the room. It’s certainly not something you want to tackle alone, believe me.
Factors Influencing Withdrawal Severity
The duration and intensity of withdrawal symptoms aren’t some arbitrary roll of the dice. They largely depend on a complex interplay of factors:
- Type of Opioid: Short-acting opioids like heroin or prescription painkillers (e.g., oxycodone, hydrocodone) tend to produce more acute and intense, but shorter-lived, withdrawal symptoms, often kicking in within 6-12 hours of the last dose. Longer-acting opioids, such as methadone or extended-release formulations, might have a delayed onset, sometimes 24-72 hours, but their withdrawal can be more protracted, lasting weeks.
- Duration and Dosage of Use: Generally, the longer you’ve used opioids and the higher the doses you’ve taken, the more severe and prolonged your withdrawal symptoms are likely to be. Your body just has more adapting to do.
- Individual Physiology: Everyone’s body processes substances differently. Metabolism, genetics, and overall physical health play a significant role. What’s a moderate withdrawal for one person could be excruciating for another.
- Co-occurring Health Conditions: Underlying physical ailments or mental health conditions, like depression or anxiety, can complicate and intensify the withdrawal experience, making it harder to manage.
The Withdrawal Timeline: Acute vs. PAWS
While acute withdrawal symptoms typically begin within hours and can last several days to a couple of weeks, that’s often just the first phase. Many people then enter what’s known as Post-Acute Withdrawal Syndrome, or PAWS. This can involve more subtle, but persistent, psychological and emotional symptoms like mood swings, anxiety, depression, difficulty sleeping, low energy, and problems with concentration. PAWS can linger for months, even a year or more, and understanding this longer arc is crucial for sustainable recovery. It certainly isn’t a straight line, recovery, not at all.
It’s absolutely paramount to consult with a healthcare professional before attempting to detox. They can use tools like the Clinical Opiiate Withdrawal Scale (COWS) to assess your symptoms and develop a personalized plan, making this initial, challenging phase as safe and manageable as possible. Trying to go it alone, frankly, is not only incredibly difficult but also quite risky. Dehydration, electrolyte imbalances, and severe psychological distress can be serious consequences. And the risk of relapse, often leading to accidental overdose due to reduced tolerance, is significantly higher without medical supervision. You really don’t want to play guessing games with your health here.
Seeking Professional Help: The Non-Negotiable First Step
Alright, so we’ve established that attempting to quit opioids without some form of medical supervision is, in essence, trying to climb Mount Everest barefoot. It’s extraordinarily risky and dramatically lowers your chances of long-term success. But why is professional help so crucial? It’s not just about getting through withdrawal; it’s about establishing a structured, medically-sound plan that’s tailored precisely to your unique needs, thereby ensuring your safety and giving you the very best shot at a sustainable recovery.
Think about it: a healthcare provider, whether it’s an addiction specialist, a general practitioner with expertise in OUD, or a team at a dedicated treatment center, brings a wealth of knowledge and resources to the table. They’re not just handing out pills; they’re assessing your physical health, your mental well-being, your history of substance use, and even your social environment. This initial assessment is foundational, laying the groundwork for a treatment plan that addresses not just the addiction itself, but any underlying issues that may be fueling it. Sarah’s journey highlights this perfectly. She told me she’d tried quitting on her own more times than she could count, only to be pulled back in by the sheer intensity of the withdrawal or the overwhelming cravings. It wasn’t until she finally reached out for professional support that things really started to shift. She needed that structure, that expert guidance, and honestly, a feeling that someone competent was truly in her corner.
Levels of Care: Finding Your Fit
Professional help isn’t a one-size-fits-all proposition. There’s a spectrum of care designed to meet varying needs and severities of OUD:
- Medical Detoxification: This is typically the first step, where medical professionals manage withdrawal symptoms in a safe, supervised environment. It can be inpatient or outpatient, depending on the severity of dependence and individual circumstances. It’s crucial for stabilizing your body and minimizing discomfort.
- Inpatient/Residential Treatment: Here, you live at a facility for a period (weeks to months), receiving intensive therapy, medical care, and structured support around the clock. It’s ideal for those with severe OUD, co-occurring mental health issues, or those who need to remove themselves from a high-risk environment.
- Intensive Outpatient Programs (IOP) / Partial Hospitalization Programs (PHP): These offer a high level of structured therapy and support during the day or evening, allowing you to live at home. PHPs are more intensive than IOPs, often running for several hours a day, several days a week, providing a bridge between inpatient and less intensive care.
- Outpatient Treatment: This involves regular therapy sessions and medication management while you continue to live at home and manage your daily responsibilities. It’s suited for those with less severe dependence or as a step-down from more intensive programs.
The key is finding the right level of care for you. A healthcare professional will help assess this, ensuring you get the comprehensive support you need to build a solid foundation for recovery.
Medication-Assisted Treatment (MAT): A Cornerstone of Modern Recovery
Let’s talk about Medication-Assisted Treatment, or MAT. This isn’t just some newfangled idea; it’s a scientifically-proven approach that marries medications with counseling and behavioral therapies. For far too long, there was this misconception, this almost puritanical belief, that true recovery meant enduring suffering and ‘toughing it out’ without any medical aid. That’s simply not true, and honestly, it’s a dangerous myth that keeps people from getting the help they desperately need. MAT isn’t trading one addiction for another; it’s a legitimate, effective medical treatment for a chronic disease. It helps stabilize your brain chemistry, which has been profoundly altered by opioid use, and significantly reduces the intense cravings and withdrawal symptoms that often drive relapse.
Think of it like treating diabetes with insulin or high blood pressure with medication. You wouldn’t tell someone with a chronic illness to just ‘willpower’ their way out of it, would you? OUD is a brain disease, and medication can be a powerful tool in its management.
The Key Players in MAT
There are three primary medications used in MAT, each with its unique mechanism of action and suitability for different individuals:
-
Methadone: This is a full opioid agonist, meaning it activates the same opioid receptors in the brain as illicit opioids, but without producing the same euphoric ‘high’ when taken as prescribed. It effectively blocks withdrawal symptoms and reduces cravings. The downside, if you can call it that, is that it’s highly regulated; methadone must be dispensed daily at a certified Opioid Treatment Program (OTP) clinic. This can be a barrier for some, demanding a significant time commitment, but for many, it provides the stability and structure needed for recovery, allowing them to rebuild their lives. It has a long half-life, providing sustained relief from cravings throughout the day.
-
Buprenorphine (often combined with Naloxone, as in Suboxone, Subutex, Zubsolv): This medication is a partial opioid agonist. What does that mean? It partially activates opioid receptors, enough to alleviate withdrawal symptoms and cravings, but it has a ‘ceiling effect’—meaning, past a certain dose, its opioid effects don’t increase, which lowers its potential for misuse and overdose. The combination with naloxone (an opioid antagonist) is designed to deter injection or snorting, as it would precipitate immediate withdrawal. Buprenorphine is incredibly versatile; it can be prescribed in a doctor’s office by certified physicians, making it much more accessible than methadone. It comes in various forms: sublingual films or tablets, and even long-acting injectables like Sublocade or implants like Probuphine, which can be a game-changer for adherence. Sarah, for instance, was prescribed buprenorphine. She recounted how it was a ‘lifesaver’, providing the necessary stability to manage cravings and step away from the daily preoccupation with using. ‘It quieted the noise in my head,’ she once told me, ‘giving me space to actually think about recovery, not just surviving the next hour.’
-
Naltrexone (Vivitrol, ReVia): Unlike methadone or buprenorphine, naltrexone is an opioid antagonist. This means it completely blocks opioid receptors, preventing opioids from having any effect. If someone on naltrexone uses an opioid, they won’t feel the ‘high,’ thereby reducing the incentive to use. It doesn’t treat withdrawal symptoms or cravings directly, so you must be opioid-free for 7-14 days (depending on the opioid used) before starting naltrexone, to avoid precipitating acute withdrawal. It comes in daily oral pill form (ReVia) or a once-monthly injectable (Vivitrol). Vivitrol, in particular, can be excellent for individuals who have already detoxed and are looking for a non-opioid, non-addictive option that provides a strong deterrent against relapse.
MAT is about offering choice and personalized care. It’s not about replacing one drug with another; it’s about using evidence-based medicine to help normalize brain function, reduce harm, and allow individuals to engage more fully in counseling and therapy. It truly gives you a fighting chance.
Behavioral Therapies: Rewiring the Brain’s Pathways
Medication is a powerful ally, no doubt, but it’s only one piece of the puzzle. To truly build a resilient, fulfilling life in recovery, you absolutely need to address the psychological underpinnings of addiction. That’s where behavioral therapies come into play, helping you unravel the complex thoughts, feelings, and behaviors that have contributed to your opioid use. These therapies are about rewiring the brain, developing robust coping strategies, and ultimately building a support network that will sustain you long after formal treatment ends.
Think of it as learning a new operating system for your brain. The old one was glitchy, prone to crashing, and certainly wasn’t serving you well. Therapy helps you install a healthier, more effective one.
Key Therapeutic Approaches:
-
Cognitive-Behavioral Therapy (CBT): This is a widely used and incredibly effective therapy. At its core, CBT helps you identify negative or distorted thought patterns and beliefs that might lead to drug use. It teaches you how these thoughts influence your feelings and behaviors. For instance, if you constantly think ‘I’m a failure, I can’t cope,’ CBT helps you challenge that thought, replace it with something more realistic, and then develop actionable strategies to handle stress or cravings without resorting to opioids. You learn practical skills like trigger identification, stress management techniques, refusal skills, and strategies for dealing with high-risk situations. Sarah found CBT particularly insightful. She realised how much of her using was linked to specific emotional triggers, like feeling overwhelmed at work or experiencing loneliness. CBT gave her concrete tools, she said, ‘like a mental toolkit,’ to handle those feelings in healthier ways, such as calling a trusted friend or going for a long walk when stress mounted.
-
Contingency Management (CM): This approach is all about positive reinforcement. It’s built on the principle that people are more likely to change their behavior if they’re rewarded for doing so. In CM, individuals receive tangible rewards (like vouchers for healthy items, gift cards, or even small cash incentives) for desired behaviors, most commonly for negative drug tests. It’s particularly effective in the early stages of recovery when motivation might still be wavering, providing immediate, tangible benefits for abstinence. It certainly offers a powerful nudge in the right direction.
-
Motivational Interviewing (MI): If you’ve ever felt stuck between wanting to change and feeling too daunted to actually do it, MI might be the right fit. It’s a collaborative, client-centered approach that helps you explore and resolve your ambivalence about change. Instead of direct confrontation, the therapist uses empathy and careful questioning to help you articulate your own reasons for wanting to recover, tapping into your intrinsic motivation. It’s a gentle yet profound way to build commitment to recovery.
-
Family Therapy/Counseling: Addiction doesn’t happen in a vacuum; it profoundly impacts families. Family therapy can be incredibly beneficial, helping loved ones understand OUD, heal old wounds, improve communication, and establish healthy boundaries. It turns the family into a support system rather than a source of potential stress or unintentional enablement.
-
Group Therapy: There’s immense power in shared experience. Group therapy sessions provide a safe space where individuals can share their struggles, successes, and insights with peers who understand what they’re going through. It fosters a sense of community, reduces feelings of isolation, and offers different perspectives on coping strategies. You learn from others, and you realize you’re not alone in your specific challenges.
These therapies, often used in combination, are vital for developing self-awareness, building resilience, and equipping you with the internal resources needed to navigate the complexities of life in recovery. They truly teach you how to live well, without opioids.
The Power of Support Systems: Building Your Tribe
Think about any major challenge in life, from running a marathon to starting a new business. No one truly conquers it alone, do they? Recovery from opioid addiction is no different. In fact, perhaps more than any other journey, it thrives on connection. Engaging with robust support systems provides a vital sense of community, shared experience, and accountability that can be absolutely indispensable. It’s about finding your tribe, the people who get it, who’ve been there, or who simply stand by you unconditionally.
Types of Support:
-
12-Step Programs (Narcotics Anonymous – NA, Alcoholics Anonymous – AA for dual diagnosis): These are perhaps the most widely known and accessed support groups, and for good reason. NA, specifically, provides a structured program for recovery based on principles of anonymity, peer support, and spiritual growth (though not necessarily religious). Sharing stories and challenges with others who understand the unique struggle of addiction can be incredibly comforting and profoundly motivating. The meetings offer a safe space to be vulnerable, to learn from others’ mistakes and successes, and to find a sense of belonging. Sarah found immense solace in NA meetings. She told me, ‘It was like finally coming home. For so long, I felt like an alien, totally isolated in my struggle. But in those rooms, everyone just got it. No judgment, just understanding.’ She found a sponsor there too, an older woman named Maria, who became a crucial mentor, a steady voice of reason when cravings hit or doubts crept in.
-
Beyond 12-Step: For those who may not resonate with the 12-Step model, there are other fantastic secular alternatives. SMART Recovery (Self-Management and Recovery Training) focuses on self-empowerment and uses cognitive behavioral therapy (CBT) tools. Refuge Recovery integrates Buddhist principles for a mindfulness-based approach. The point is, explore until you find a philosophy that truly resonates with you.
-
Family and Friends: Rebuilding trust and open communication with loved ones can be a long process, but their support is invaluable. Educating your family about OUD and recovery can transform them into powerful allies. A strong, understanding home environment can make all the difference.
-
Sponsors and Mentors: In 12-Step programs, a sponsor is someone who has more experience in recovery and guides you through the steps. But beyond that, finding any positive mentor—someone who embodies the kind of healthy, sober life you aspire to—can provide invaluable wisdom and encouragement.
-
Online Communities: The digital age offers new avenues for support. Online forums and recovery communities can provide a convenient, anonymous space to connect, share, and receive encouragement, especially if in-person meetings are difficult to access. Always ensure these communities are moderated and promote healthy recovery principles.
Building a robust support network isn’t about being weak; it’s about being smart. It’s recognizing that human connection is a fundamental need, and when harnessed for recovery, it becomes an incredibly powerful force.
Self-Care and Lifestyle Changes: Nurturing Your Whole Self
Okay, so you’ve got the professional help sorted, maybe you’re on MAT, and you’re diving into therapy and finding your support tribe. That’s a phenomenal start. But here’s the thing: recovery isn’t just about stopping drug use; it’s about rebuilding a life worth living, one that’s fulfilling, joyful, and resilient. And a huge part of that is embracing radical self-care and making sustainable lifestyle changes. It’s about nurturing your whole self—mind, body, and spirit—and giving yourself the best possible chance to thrive. You know, you can’t pour from an empty cup, as the saying goes, and recovery often drains you before it replenishes you.
Bolstering Your Physical Health:
-
Exercise: Moving Your Way to Wellness: This isn’t just about looking good (though that’s a nice bonus!). Regular physical activity is a potent medicine for both the body and the mind. It releases endorphins, those natural mood boosters, which can help combat depression and anxiety, common companions in early recovery. Whether it’s a brisk walk, hitting the gym, cycling, swimming, or dancing, find something you genuinely enjoy. Sarah, for instance, discovered yoga. She started with gentle classes, she told me, a little skeptical at first. But soon, she found that the combination of movement, breathwork, and mindfulness not only improved her physical strength and flexibility but also provided a profound sense of mental clarity and calm. ‘It was my moving meditation,’ she’d say, ‘the hour where my brain could finally just… quiet down.’
-
Nutrition: Fueling Your Recovery: Your brain and body need proper fuel to heal and function optimally. Processed foods, excessive sugar, and caffeine can exacerbate mood swings and energy crashes. Focus on a balanced diet rich in whole foods: lean proteins, healthy fats, plenty of fruits and vegetables, and whole grains. Hydration is also key—drink plenty of water throughout the day. A healthy gut often means a healthier mind, so consider probiotics or fermented foods to support your gut microbiome.
-
Sleep Hygiene: The Unsung Hero: Sleep deprivation can be a major trigger for cravings and mood instability. Prioritize getting 7-9 hours of quality sleep each night. Establish a calming bedtime routine: dim lights, avoid screens at least an hour before bed, listen to soothing music, or read. Your body does its best healing and repair while you’re asleep; don’t underestimate its power.
Cultivating Mental & Emotional Well-being:
-
Mindfulness and Meditation: Learning to be present, without judgment, can profoundly impact your ability to manage cravings, anxiety, and stress. Simple breathing exercises, guided meditations, or body scans can help you observe difficult thoughts and feelings without being overwhelmed by them. It’s about creating space between the trigger and your reaction.
-
Journaling: Putting your thoughts and feelings down on paper can be incredibly cathartic. It’s a private space to process emotions, track your progress, identify patterns, and even vent frustrations. It gives you perspective and helps you reflect on your journey.
-
Rediscovering Hobbies and Interests: Many people in active addiction lose touch with passions they once enjoyed. Recovery is a time to rediscover those healthy outlets or explore new ones. Whether it’s playing music, painting, hiking, gardening, or volunteering, engaging in meaningful activities provides purpose, reduces boredom (a major relapse trigger!), and builds a sense of identity beyond addiction.
-
Stress Management Techniques: Life happens, and stress is inevitable. Having a toolkit of healthy stress relievers is crucial. This could include deep breathing exercises, progressive muscle relaxation, spending time in nature, listening to music, or connecting with a trusted friend. Identifying your personal stress signals and having a plan to address them proactively can make all the difference.
Embracing these self-care practices isn’t selfish; it’s absolutely essential. They are the daily acts of kindness you show yourself, the building blocks for a robust, fulfilling life in recovery.
Navigating Triggers and Preventing Relapse: Equipping Yourself for the Long Haul
So you’re building this new, healthier life, and it feels good. You’re making progress, feeling stronger, more grounded. But let’s be honest, life isn’t a straight line, and recovery certainly isn’t a one-and-done deal. There will be moments, situations, and emotions that threaten to pull you back, even just for a fleeting second. These are what we call triggers, and understanding them, preparing for them, and developing robust coping strategies is absolutely vital for preventing relapse and maintaining your hard-won sobriety. It’s like equipping yourself with a weather forecast and a sturdy umbrella before heading into a potential storm.
Understanding Your Triggers:
Triggers are anything that reminds you of using opioids or creates an urge to use. They can be incredibly varied and deeply personal. They generally fall into two main categories:
- External Triggers: These are people, places, things, or even times of day associated with past drug use. Think old using friends, specific neighborhoods or houses where you used, drug paraphernalia, certain music, or even paydays. Sarah, for instance, realized that seeing old texts from using buddies or even just walking past a particular corner store would send a jolt of anxiety and craving through her. She had to really work at identifying those specific external cues.
- Internal Triggers: These are thoughts, feelings, or physical sensations. They’re often more insidious and harder to avoid. Examples include stress, anxiety, depression, boredom, anger, loneliness, physical pain, or even feeling overly confident or euphoric (often called ‘euphoric recall’). A common one I’ve heard is the ‘restless, irritable, discontent’ feeling that can creep in when recovery feels stagnant.
Developing Your Relapse Prevention Plan:
Identifying your triggers is just the first step. The real work is in developing a comprehensive plan to cope with them, and crucially, what to do if you slip. Because, let’s face it, setbacks can happen, and they don’t erase all your progress. They’re simply learning opportunities, painful as they might be. The goal is to get back on track immediately.
Here are some key strategies:
-
Avoidance (Where Possible): This is the simplest, most direct strategy. If you know certain people, places, or situations are high-risk, avoid them. This might mean changing your route home, unfollowing certain social media accounts, or setting firm boundaries with old associates. It certainly isn’t always easy, but it’s often necessary, especially in early recovery.
-
Distraction and Redirection: When a craving hits, it can feel all-consuming. Have a list of healthy, engaging activities you can immediately turn to. Call a friend, go for a walk, listen to music, clean the house, do a puzzle, or engage in a hobby. The goal is to shift your focus and ride out the craving until it passes, which it will.
-
Coping Skills Application: This is where all that hard work in therapy pays off. Remember those CBT techniques? Practice mindfulness to observe the craving without acting on it. Use deep breathing or grounding techniques to manage anxiety. Challenge negative thoughts that might be rationalizing using.
-
Utilize Your Support Network: This is why you built your tribe! When a trigger hits, reach out immediately. Call your sponsor, a trusted friend, your therapist, or attend an impromptu meeting. Sharing your struggle aloud often diminishes its power. Sarah learned this the hard way. Early on, she’d try to battle cravings alone, which often led to intense internal struggles. But she then started calling Maria, her sponsor, or another NA member, and just talking it out. She’d always say, ‘Just hearing my own voice admitting I was struggling made the craving lose half its grip.’
-
Play the Tape Forward: When the urge to use is strong, mentally walk through the consequences of picking up again. What would happen tomorrow? The next day? How would you feel? Who would you disappoint? This powerful visualization can often short-circuit the impulsive desire.
-
Develop an Emergency Relapse Plan: Have a clear, step-by-step plan for what to do if you do relapse. Who will you call first? What medical assistance might you need? How will you re-engage with your treatment and support system? Having this plan in place reduces shame and enables immediate action, turning a slip into a temporary setback rather than a full-blown fall.
Remember, relapse is often part of the recovery journey for many, but it doesn’t mean failure. It means you’re human, and it’s an opportunity to re-evaluate, learn, and strengthen your resolve. The key is to learn from it, seek help immediately, and recommit to your path. You’ve got this.
Setting Goals and Celebrating Milestones: Fueling Your Progress
Recovery, as we’ve discussed, is a marathon, not a sprint. And just like any long-distance race, you need markers along the way to measure your progress, keep your spirits up, and remind yourself how far you’ve come. Setting achievable goals and genuinely celebrating every milestone, no matter how small, is incredibly powerful. It builds momentum, reinforces positive behaviors, and reminds you of your inherent strength and unwavering commitment. You wouldn’t expect to run a whole marathon without water breaks, would you? Celebrate your small wins, they’re your hydration stations.
The Power of Goal Setting:
- Provides Structure and Purpose: Goals give you something tangible to work towards each day. They transform an overwhelming, abstract concept like ‘recovery’ into manageable, actionable steps.
- Boosts Motivation: Successfully achieving a goal, no matter how small, releases dopamine—your brain’s natural reward chemical. This positive feedback loop motivates you to keep going.
- Builds Self-Efficacy: Each goal achieved builds your belief in your own ability to succeed. This self-confidence is crucial for long-term recovery.
Making Your Goals SMART:
For goals to be truly effective, they should be SMART:
- Specific: Instead of ‘I want to get better,’ try ‘I will attend three NA meetings this week.’
- Measurable: How will you know you’ve achieved it? ‘I will call my sponsor daily.’
- Achievable: Is it realistic given your current circumstances? Don’t set yourself up for failure.
- Relevant: Does it align with your overall recovery goals? Is it meaningful to you?
- Time-bound: Set a deadline. ‘By next Friday, I will have researched three therapists.’
Short-Term vs. Long-Term Goals:
It’s good to have both:
- Short-Term Goals: These are your daily or weekly wins. ‘Today, I will practice mindfulness for 10 minutes.’ ‘This week, I will stick to my sleep schedule.’ These build immediate confidence and consistency.
- Long-Term Goals: These are your bigger picture aspirations. ‘I will be sober for one year.’ ‘I will get a stable job.’ ‘I will repair my relationship with my family.’ These provide direction and a larger vision for your life.
The Art of Celebration:
This is where it gets fun! Don’t just tick a box; celebrate your progress. And I don’t mean celebrating with unhealthy habits. I mean finding healthy, meaningful ways to acknowledge your hard work.
- Acknowledge Small Victories: Did you get through a tough craving without using? Did you attend all your meetings? Did you reach out to someone when you felt isolated? Pat yourself on the back! Each one is a testament to your strength and commitment.
- Healthy Rewards: Treat yourself to something you enjoy: a special meal, a new book, a movie, a relaxing bath, a day trip to the beach, or a new piece of workout gear. These are positive reinforcers that connect sobriety with pleasure.
- Share Your Success: Tell your sponsor, your therapist, your supportive friends or family. Sharing your wins not only reinforces them for you but also inspires others. Sarah, bless her, really embraced this. She celebrated her one-year sobriety anniversary not with a big, flashy party (which might have been triggering anyway), but with a small, intimate gathering of her closest supportive friends and family. It was a quiet acknowledgment of her incredible hard work and progress, a moment of profound gratitude and pride. She even treated herself to a new set of art supplies, something she’d wanted for ages, a tangible symbol of reclaiming her creative spirit.
Celebrating your journey isn’t boastful; it’s essential. It reminds you that every single day sober is a powerful step forward, and that you are truly capable of amazing things.
Staying Committed and Embracing the Lifelong Journey: A Marathon, Not a Sprint
Here’s the plain truth, the one every person in long-term recovery understands: recovery isn’t a destination you arrive at and then simply stop working. It’s a continuous, evolving journey, a marathon that truly lasts a lifetime. There will be good days, great days, and yes, there will inevitably be challenging days, even setbacks. The key isn’t to be perfect; it’s to stay committed, to learn from every experience, and to relentlessly seek help when needed. You see, the person who falls isn’t the one who fails; the one who fails is the person who refuses to get back up.
Opioid Use Disorder is a chronic condition, much like diabetes or heart disease. It requires ongoing management, vigilance, and self-care. There isn’t a ‘cure’ in the traditional sense, but there is sustained remission and a return to a fulfilling, productive life. It’s about building resilience, developing coping mechanisms that become second nature, and continuously growing as an individual.
The Path Forward:
-
Embrace Resilience: Life will throw curveballs. You’ll face stress, grief, disappointment, and unexpected challenges. True resilience isn’t about avoiding these things; it’s about your capacity to bounce back, to adapt, and to grow stronger through adversity. Your recovery journey has already forged immense resilience within you, perhaps more than you even realize.
-
Continuous Learning: The landscape of recovery and self-awareness is always expanding. Stay curious. Continue attending meetings, engaging in therapy, reading self-help books, or exploring new mindfulness practices. What worked for you in early recovery might need to evolve as you do. Don’t become complacent.
-
Give Back: One of the most powerful motivators in long-term recovery for many is the opportunity to help others. Whether it’s sponsoring someone in a 12-Step program, volunteering, or simply sharing your story with someone who’s struggling, giving back reinforces your own sobriety and provides immense meaning and purpose. It’s a wonderful way to cement your own progress.
-
Self-Compassion: Be kind to yourself. You’re doing something incredibly hard and incredibly brave. There will be days you feel frustrated, tired, or just plain down. On those days, extend yourself the same grace and understanding you would offer a dear friend. Perfection isn’t the goal; progress is.
Sarah, throughout her journey, faced numerous challenges. There were job changes, relationship struggles, moments of intense grief, and even lingering health issues. She told me, ‘It felt like sometimes life just kept hitting me with everything it had.’ But she remained dedicated, consistently leaning on her support system, attending meetings, and reminding herself that each day sober wasn’t just another day without using; it was a day building a future she truly wanted, a step closer to the peace and freedom she now cherished. Her dedication was really inspiring, actually.
Remember, you’re not alone in this journey. The path to recovery is well-trodden by millions who have found their way to a life beyond opioid addiction. With the right support, the appropriate treatment, an unyielding determination, and a healthy dose of self-compassion, sustained recovery is not just possible; it’s truly within your reach. Keep going. You’ve got this.
References
-
Healthgrades. (n.d.). Recovering from Opioid Use Disorder. Retrieved from (https://resources.healthgrades.com/right-care/substance-abuse-and-addiction/opioid-use-disorder-focus-on-recovery-not-shame)
-
Healthgrades. (n.d.). 7 Tips for Overcoming Opioid Use Disorder. Retrieved from (https://www.healthgrades.com/right-care/substance-abuse-and-addiction/7-tips-for-overcoming-opioid-use-disorder)
-
Healthgrades. (n.d.). Just Started Treating Opioid Use Disorder? Know Your Medication Options. Retrieved from (https://resources.healthgrades.com/right-care/substance-abuse-and-addiction/just-started-treating-opioid-use-disorder-know-your-medication-options)
-
Healthgrades. (n.d.). Medication for Opioid Use Disorder | Treating Opioid Use Disorder. Retrieved from (https://resources.healthgrades.com/right-care/substance-abuse-and-addiction/medication-for-opioid-use-disorder-what-works-best-for-your-schedule)
-
Healthgrades. (n.d.). Going Through Opioid Use Disorder Withdrawal with Medication. Retrieved from (https://www.healthgrades.com/right-care/substance-abuse-and-addiction/going-through-opioid-use-disorder-withdrawal-with-medication)
-
Healthgrades. (n.d.). How to Find the Right Opioid Use Disorder Treatment for You. Retrieved from (https://www.healthgrades.com/right-care/substance-abuse-and-addiction/how-to-find-the-right-opioid-use-disorder-treatment-for-you)
-
Wikipedia. (n.d.). Opioid Use Disorder. Retrieved from (https://en.wikipedia.org/wiki/Opioid_use_disorder)
-
Wikipedia. (n.d.). Clinical Opiate Withdrawal Scale. Retrieved from (https://en.wikipedia.org/wiki/Clinical_Opiate_Withdrawal_Scale)


Be the first to comment