Navigating the Fentanyl Tempest: Charting a Course for Innovative Recovery
The fentanyl crisis, you know, it isn’t just a headline anymore; it’s a relentless storm, a national emergency that’s battering communities, tearing through families, and leaving an unthinkable trail of devastation. Frankly, our traditional approaches, while absolutely vital, sometimes feel like a single life raft against a tsunami. They’re good, they’re necessary, but they often struggle to truly grapple with the sheer, insidious complexity of modern opioid dependence. That’s why we’re seeing this incredible surge, this new wave of programs emerging from the wreckage, deftly weaving together cutting-edge technology, profound holistic therapies, and the bedrock of community support. These aren’t just minor tweaks; they’re comprehensive solutions, blueprints for a genuinely robust path to sobriety for those caught in fentanyl’s grip.
Think about it for a moment. This isn’t just about treating a physical dependence; it’s about addressing a profound disruption of mind, body, and spirit, often compounded by deep-seated trauma and societal pressures. We need tools that aren’t just reactive, but proactive. We need support that isn’t just clinical, but deeply human. And we’re beginning to see exactly that take shape, which honestly, is incredibly encouraging.
The Digital Horizon: Technological Innovations Reimagining Recovery
It’s hardly a surprise, is it? In our hyper-connected digital age, technology isn’t just a nice-to-have; it’s a pivotal, transformative force in addiction treatment. It’s helping us bridge gaps, personalize care, and even predict potential dangers before they fully materialize. We’re talking about innovations that would’ve seemed like science fiction just a decade ago.
Take mobile applications, for instance. Apps like ‘Addict Free’ are truly revolutionizing relapse prevention, employing sophisticated algorithms to analyze spatial and temporal factors. What does that mean? Well, it means the app might learn that you, say, tend to experience stronger cravings when you’re in a particular neighborhood at a certain time of day, or after receiving specific social media notifications. It then uses that data, crunching immense amounts of user profiles, historical relapse patterns, and environmental cues to try and predict and, crucially, prevent a relapse before it even fully takes hold. These aren’t passive tools. They’re dynamic, providing real-time coping strategies right there in your pocket, making support accessible anytime, anywhere. Imagine having a personalized crisis coach whispering encouragement and strategies the moment you feel that old familiar pull. It’s a game-changer, isn’t it? It democratizes access to immediate, personalized support, reducing the often-paralyzing barrier of having to reach out to another human during a moment of profound vulnerability.
But the innovation doesn’t stop there. Wearable biosensors are moving from the realm of academic papers into practical application. These aren’t just fancy fitness trackers, mind you. We’re talking about devices that continuously monitor vital signs with remarkable precision. They’re looking at subtle shifts in breathing patterns, heart rate variability, skin conductance, even oxygen saturation levels – the very indicators that scream ‘danger’ when an opioid overdose begins to take hold. The moment these sensors detect the tell-tale signs of respiratory depression or a dangerously slowing heart rate, they’re designed to immediately alert emergency responders, or perhaps a designated loved one. This proactive approach to overdose prevention could, frankly, save countless lives. It’s like having an invisible guardian angel keeping watch, ready to sound the alarm when seconds truly count. And think of the peace of mind that offers to families, knowing there’s an added layer of protection.
And we can’t forget telehealth and virtual care. For too long, geographical barriers have prevented so many from accessing critical treatment. If you live in a rural community, getting to an addiction specialist or even a regular therapy session can mean hours of driving, lost wages, and childcare nightmares. Telehealth obliterates those barriers. Suddenly, expert therapy sessions, crucial medication-assisted treatment (MAT) consultations, and supportive group therapy are just a video call away. This doesn’t just offer convenience; it ensures continuity of care, which is absolutely vital in recovery. The challenge, of course, lies in ensuring everyone has adequate broadband access and digital literacy, but the potential to expand the reach of life-saving services is just immense.
Then there’s the exciting, somewhat futuristic realm of Virtual Reality (VR) and Augmented Reality (AR). You might think of VR for gaming, but in addiction treatment, it’s being used to simulate high-risk environments in a completely safe, controlled setting. Imagine a person in recovery being able to practice refusing drugs at a simulated party, or navigating a street corner where they once used, all without the actual risk of relapse. This ‘exposure therapy’ in a virtual space allows individuals to build crucial coping skills, manage cravings, and rehearse challenging social interactions. It builds muscle memory for sobriety. AR, on the other hand, could offer real-time information overlays in daily life – perhaps a gentle prompt on your phone screen when you approach a high-risk location, reminding you of your coping strategies, or even displaying personalized motivational messages. It’s about creating an immersive, interactive training ground for life after addiction, which really, is pretty incredible.
Nurturing the Whole Self: Holistic Therapies for Comprehensive Healing
Moving beyond the technological marvels, there’s a profound shift towards holistic therapies, acknowledging that addiction isn’t just a physical ailment. It’s a deep-seated disruption that affects the mind, body, and spirit. This isn’t some new-age fad; it’s a science-backed recognition that true healing requires a multi-faceted approach. Programs that thoughtfully incorporate mindfulness, meditation, and physical activities aren’t just adding ‘extras’; they’re addressing the fundamental imbalances that often fuel addiction, fostering overall well-being and resilience.
Mindfulness practices, for instance, teach individuals to observe their thoughts and feelings without judgment, creating a crucial pause between a craving and a reactive behavior. This can be incredibly empowering. Meditation helps calm the nervous system, reducing anxiety and stress, which are often major triggers for substance use. And physical activities – yoga, hiking, tai chi, even just a brisk walk – release endorphins, improve mood, and provide a healthy outlet for pent-up energy and stress. I’ve heard countless stories of people finding solace and strength in these practices. A friend of mine, struggling for years, finally found her footing when she discovered a yoga practice tailored for recovery. She’d tell me, ‘It’s not just about the poses; it’s about learning to breathe through discomfort, just like I have to do with cravings.’ It truly is about retraining the brain, promoting neuroplasticity, and restoring those vital dopamine pathways that addiction hijacks.
Eye Movement Desensitization and Reprocessing (EMDR) therapy is another profoundly impactful approach, particularly effective for individuals with histories of trauma. And let’s be honest, the overlap between trauma and addiction is staggering. EMDR helps individuals reprocess traumatic memories, essentially reducing their emotional charge. It’s not about erasing the memory, but about allowing the brain to store it in a way that doesn’t trigger the same intense distress, anxiety, or flashbacks. For someone who might have turned to fentanyl to numb the unbearable pain of past trauma, EMDR offers a pathway to truly heal those wounds, making sustained recovery far more attainable. It’s like untangling a knotted rope inside someone’s mind, allowing them to finally breathe freely.
But the holistic journey extends further. We’re seeing a growing emphasis on nutritional support, recognizing the profound connection between what we eat and our mental well-being. The emerging science of the gut-brain axis is illuminating how a healthy gut microbiome can impact mood, energy levels, and even susceptibility to cravings. Personalized nutrition plans, designed to restore nutrient deficiencies and support brain health, are becoming an integral part of comprehensive recovery programs. It’s not just about calorie counting; it’s about feeding the very systems that addiction has starved and disrupted. Think of it as rebuilding the body’s internal architecture, brick by healthy brick.
And let’s not overlook ancient practices like acupuncture and Traditional Chinese Medicine (TCM). While perhaps not as mainstream, they’re gaining significant traction for their ability to alleviate withdrawal symptoms, reduce anxiety, and manage chronic pain – a common precursor to opioid use. Auricular acupuncture, specifically, involving tiny needles in the ear, has shown promising results in calming the nervous system and easing cravings. These practices offer complementary avenues for healing, tapping into wisdom developed over centuries to support the body’s innate ability to heal. It’s a testament to the idea that sometimes, the oldest paths can lead to the newest breakthroughs in wellness.
The Human Connection: Community Support and Peer Involvement as Pillars of Recovery
For all the cutting-edge tech and profound therapies, community support remains an absolute cornerstone of successful recovery. You simply can’t underestimate the power of human connection, of feeling truly seen and understood. We’re social creatures, after all, and addiction often thrives in isolation. Peer support programs, like the ‘NSPIRED Peer Support App for Teens in Recovery,’ provide incredible platforms for individuals to share their lived experiences, offer genuine encouragement, and build that invaluable sense of belonging. It’s a space where judgment melts away, replaced by empathy and shared understanding.
These programs go far beyond just apps, though. We’re seeing a flourishing of recovery community centers, where people can connect, attend meetings, and simply exist in a supportive, sober environment. Peer navigators, individuals who have walked the path of recovery themselves, act as guides, offering practical advice and emotional support, helping newcomers navigate the often-complex world of treatment and reintegration. The psychology here is potent: when you hear someone say, ‘I’ve been where you are, and I made it through,’ it instills a sense of hope that clinical advice alone often can’t replicate. It’s about solidarity, about knowing you’re not walking this challenging road alone. It fosters a collective resilience that’s truly awe-inspiring.
Family involvement, too, is absolutely crucial. Addiction doesn’t happen in a vacuum; it impacts the entire family system. Programs that educate and actively engage family members are vital for rebuilding trust, fostering healthy communication patterns, and setting boundaries that are supportive rather than enabling. This isn’t always easy, of course. There’s often deep pain, resentment, and misunderstanding to unpack. But through family therapy models, like Multidimensional Family Therapy (MDFT), families learn to function more cohesively, creating an environment where the individual in recovery feels truly supported, not scrutinized. It’s about healing the family unit as a whole, because sustained sobriety often depends on a stable, understanding home base. Without that, it’s an uphill battle.
Then there’s the often-overlooked but utterly critical link between stable housing, meaningful employment, and sustained recovery. It’s a tough truth: it’s incredibly difficult to focus on healing when you don’t know where you’ll sleep at night or how you’ll put food on the table. This is where recovery housing models, from structured sober living environments to independent recovery-focused apartments, become so essential. They provide a safe, drug-free space to rebuild. Similarly, job training programs, vocational counseling, and support for reintegrating into the workforce give individuals purpose, financial stability, and a sense of dignity. These aren’t just ‘add-ons’; they are foundational elements that allow individuals to reclaim their lives and contribute meaningfully to society. It’s about building a new life, not just stopping drug use.
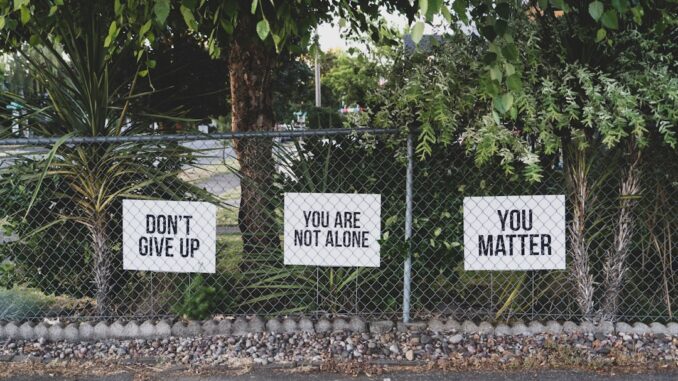
And we can’t talk about community without addressing the pervasive stigma associated with addiction. It’s a quiet killer, often preventing people from seeking help or pushing them back into the shadows. Community initiatives that actively combat this stigma – through public awareness campaigns, using person-first language (e.g., ‘person with a substance use disorder’ instead of ‘addict’), and sharing stories of successful recovery – are incredibly powerful. They chip away at the misconceptions, fostering a more compassionate and understanding society where seeking help is normalized, not shamed. We have to keep reminding people: addiction is a disease, not a moral failing. You wouldn’t shame someone for having cancer, so why addiction? It’s a question worth pondering.
Mitigating Harm, Paving Paths: Integrating Harm Reduction Strategies
Harm reduction isn’t about enabling drug use; it’s about meeting people where they are, acknowledging the immediate dangers, and providing a critical bridge to recovery-oriented services. When facing a crisis as deadly as fentanyl, immediate safety measures are paramount. And these strategies, once controversial, are increasingly recognized as pragmatic, life-saving interventions.
Supervised consumption facilities (SCFs), sometimes called overdose prevention sites, are a prime example. These are safe, hygienic spaces where individuals can consume pre-obtained drugs under the supervision of trained medical staff. The primary goal is to prevent overdose deaths – staff are on hand with naloxone, ready to intervene instantly – but they also reduce the transmission of infectious diseases like HIV and Hepatitis C through clean supplies. Crucially, SCFs also serve as crucial access points, connecting users to vital treatment programs, housing services, and other social supports they might never have otherwise encountered. They’re not just a place to use; they’re a beacon of hope, a starting point for change, even if it feels small at first glance. They say, ‘We see you, and your life matters.’
Similarly, syringe service programs (SSPs) play a vital role. They don’t just provide clean needles and syringes, but also facilitate safe disposal of used equipment, offer naloxone distribution and training, and provide testing for infectious diseases. They are a frontline public health intervention, drastically reducing the spread of blood-borne infections that otherwise plague communities affected by injection drug use. It’s about reducing suffering, plain and simple.
And speaking of naloxone, its widespread distribution is an absolute necessity. You know it as Narcan, that powerful opioid overdose reversal medication. Training first responders, family members, and even the general public on how to administer it means that someone having an overdose doesn’t have to die waiting for an ambulance. Equipping communities with this tool is literally putting life-saving power into the hands of ordinary people. It’s incredible to witness how quickly it can bring someone back from the brink.
Fentanyl test strips are another innovative harm reduction tool gaining traction. These small, inexpensive strips empower users to test their illicit drug supply for the presence of fentanyl, which is often mixed into other drugs without the user’s knowledge. This allows individuals to make more informed decisions about their use, potentially preventing accidental overdose. While there have been debates around their legality and perceived ‘encouragement’ of drug use, the reality is they save lives by providing critical information in a landscape saturated with deadly, unpredictable substances. It’s not about condoning drug use, it’s about preventing death from poisoned drugs.
And we absolutely must include Medication-Assisted Treatment (MAT) here, because it’s arguably the most critical harm reduction and recovery tool we possess. Medications like buprenorphine, methadone, and naltrexone aren’t just about managing withdrawal; they drastically reduce cravings, stabilize brain chemistry, and significantly lower the risk of overdose. When combined with counseling and behavioral therapies, MAT is proven to be the most effective treatment for opioid use disorder. There’s often this persistent misconception, isn’t there, that it’s ‘trading one addiction for another.’ But that’s simply not true. It’s about treating a chronic brain disease with evidence-based medicine, allowing individuals to stabilize and engage in meaningful recovery. It’s time we fully embraced it without reservation.
The Unfolding Story: Challenges and Opportunities Ahead
The path forward isn’t without its hurdles, of course. For all these incredible innovations, we face significant challenges that demand sustained attention and bold action. Policy and funding, for instance, are massive pieces of the puzzle. We need consistent, substantial government funding for treatment, prevention, and harm reduction initiatives. Furthermore, policy changes are desperately needed to expand access to MAT, to reconsider punitive drug laws, and to better integrate mental health and substance use disorder treatment into our broader healthcare system. It’s a complex legislative dance, but one we simply can’t afford to get wrong.
Inter-agency collaboration is another crucial factor. We can’t have healthcare working in one silo, law enforcement in another, and social services completely separate. Effective solutions demand that these disparate entities work together seamlessly, sharing information and coordinating efforts. Imagine a system where a person encountered by law enforcement for a drug-related offense is immediately connected with treatment options, rather than simply incarcerated. That’s the kind of integrated approach we need to strive for, a truly holistic societal response.
And let’s not forget the continuous need for robust research and data collection. We need to keep refining our understanding of addiction, identifying what truly works, and adapting our strategies based on evidence. This ongoing scientific inquiry will ensure that our interventions are not just well-intentioned, but maximally effective.
Finally, the future points towards an exciting frontier: personalized medicine for addiction. Just as we tailor cancer treatments to an individual’s genetic makeup, we’re moving towards a time when addiction treatment plans can be customized based on an individual’s unique genetics, co-occurring mental health conditions, personal preferences, and even their specific brain chemistry. This bespoke approach promises to significantly enhance treatment outcomes, making recovery not just possible, but more sustainable for each unique individual.
The Resilient Horizon: A Comprehensive Path to Recovery
The fentanyl crisis, in its profound devastation, has underscored a stark reality: we can’t afford to be complacent. It demands not just a response, but a truly multifaceted, dynamic, and empathetic one. By wholeheartedly embracing technological innovations – from predictive apps to life-saving biosensors – by nurturing the whole person through profound holistic therapies, and by strengthening the foundational bedrock of community support and smart harm reduction strategies, we are building a genuinely comprehensive path to recovery.
This isn’t a quick fix, you see. It’s a marathon, not a sprint, a monumental undertaking that requires sustained effort, unwavering compassion, and a willingness to innovate at every turn. But by investing in these forward-thinking strategies, we’re not just addressing the immediate, terrifying dangers of addiction; we’re laying down the robust groundwork for sustained sobriety, improved quality of life, and ultimately, a more resilient, healthier society. And that, my friends, is a future worth fighting for, isn’t it?


Be the first to comment