Florida’s Compassionate Embrace: A Deep Dive into Support for Our Serving Heroes
Florida, a state with a proud tradition of supporting its service members, has recently stepped up in a monumental way. They’ve rolled out a truly comprehensive program, dedicated squarely to assisting veterans and first responders as they battle the insidious grip of addiction. It’s more than just a recovery initiative, you know? It’s a profound acknowledgment of the unique, often invisible, struggles these incredible individuals face, designed to foster their recovery and, ultimately, their profound well-being.
Think about it: who among us truly understands the weight of a life-or-death decision, the split-second choices that haunt you for years, or the sheer, relentless exposure to trauma? Not many. This program, then, isn’t just another box-ticking exercise; it’s a testament to understanding, to empathy, and to giving back to those who’ve given so much.
Unmasking the Invisible Wounds: Why Specialised Care Matters
Veterans and first responders, they’re not just ‘high-stress professions’. It’s a lifestyle, a calling, that continuously exposes them to situations that would break most of us. The constant hum of danger, the horrific scenes, the crushing responsibility – these experiences don’t just fade away with time. They embed themselves, sometimes quite deeply, leading to a complex web of mental health challenges, and, quite often, substance use disorders. It’s almost an understandable, albeit destructive, coping mechanism, isn’t it?
The Lingering Shadows of Trauma
Consider a young Marine, fresh out of a combat zone, returning to the seemingly mundane rhythm of civilian life. He’s probably spent months, maybe years, on high alert, his senses finely tuned to threat. Now, back home, the silence is deafening, the lack of immediate purpose disorienting. That sense of camaraderie, the unbreakable bonds forged in shared adversity, is suddenly gone, replaced by a quiet isolation. It’s tough, really tough, to just ‘switch off’ that survival mode. For many, that disjunction, the emotional whiplash, can lead to overwhelming feelings of anxiety, depression, and a profound sense of loneliness. When the internal noise becomes too much, sadly, a bottle or a pill often seems like the quickest path to silence it, if only for a little while.
Similarly, imagine the daily grind of a seasoned paramedic. One moment, they’re resuscitating a child, the next, they’re extricating bodies from a mangled car wreck, then comforting a grieving family. Day in, day out, they witness humanity at its most vulnerable, its most tragic. This isn’t just stress; it’s chronic, cumulative trauma. It chips away at you, slowly but surely, until you might not even recognise the person staring back from the mirror. Compassion fatigue sets in, certainly, and for some, it morphs into a heavier burden: moral injury, the psychological distress from actions or inactions that violate one’s deeply held moral beliefs. They see, and often internalise, so much suffering, and without proper outlets, the pressure can build to an unbearable point. So, it’s no surprise that some might turn to substances just to numb the sharp edges of their memories, to find even a moment of peace from the relentless replay of horrors.
What’s particularly challenging for these groups, you see, is the inherent culture of stoicism. There’s this unspoken expectation that you’re strong, resilient, impervious to pain. A firefighter can’t show fear, a police officer can’t break down, a soldier can’t admit weakness. This ‘mask’ they wear, while necessary for their operational duties, becomes a huge barrier to seeking help. Admitting you’re struggling, admitting you might have an addiction, it can feel like a betrayal of everything you stand for, a personal failure. This pervasive stigma, sadly, often keeps people suffering in silence, pushing them deeper into the shadows of substance misuse.
The Program’s Blueprint: A Multi-faceted Approach to Healing
The beauty of Florida’s newly launched program isn’t just its existence, but its truly holistic, well, holistic design. It moves beyond a one-size-fits-all model, recognising that a veteran with PTSD might need different interventions than a first responder dealing with the aftermath of a critical incident. It’s tailored, it’s thoughtful, and it’s comprehensive. And that’s what makes it so potentially impactful, don’t you think?
Comprehensive Assessment: Peeling Back the Layers
Recovery, genuine recovery, starts with understanding. So, the program kicks off with an incredibly thorough, multi-faceted assessment. It’s not just a quick chat; individuals undergo extensive evaluations, often involving a multidisciplinary team of clinicians—psychiatrists, psychologists, addiction specialists, social workers. They’re looking for the whole picture: their unique challenges, the depth of their substance use history, and crucially, any co-occurring mental health disorders like depression, anxiety, or post-traumatic stress disorder. They use clinical interviews, psychological testing, and sometimes even neurocognitive assessments to really map out the landscape of their needs. This deep dive ensures that the subsequent treatment isn’t just guessing, it’s precision-guided.
Tailored Treatment Plans: The Road Map to Recovery
Once the assessment paints a clear picture, a personalised treatment plan comes into focus. And this is where the evidence-based therapies really shine, offering practical, proven paths to healing. We’re talking about things like:
- Cognitive Behavioral Therapy (CBT): This helps individuals identify and challenge negative thought patterns that contribute to substance use. It’s about retraining the mind, building resilience.
- Dialectical Behavior Therapy (DBT): Particularly useful for emotional regulation and distress tolerance, helping individuals manage intense feelings without resorting to substances.
- Eye Movement Desensitization and Reprocessing (EMDR): A powerful therapy for processing traumatic memories, effectively reducing their emotional charge. Imagine the relief of having a horrific memory lose its power over you.
- Trauma-Informed Care: This is less a specific therapy and more an overarching philosophy. It ensures that the entire treatment environment understands the pervasive impact of trauma and avoids re-traumatizing individuals. It’s about safety, trustworthiness, peer support, collaboration, and empowerment.
But it doesn’t stop there. The plans also often integrate medication-assisted treatment (MAT) when appropriate, recognising that for many, pharmacological support can significantly aid in managing cravings and preventing relapse. Moreover, it’s a holistic approach, considering physical health, nutrition, even spiritual well-being. Individuals also learn crucial coping skills, emotion regulation techniques, and healthier communication strategies, essential tools for navigating life without relying on substances. It’s about equipping them for the long haul.
Peer Support Networks: The Power of Shared Journeys
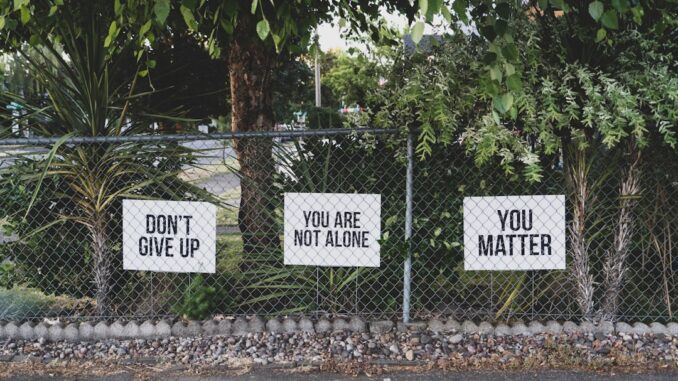
There’s an undeniable, almost magical, power in connection, isn’t there? This program strongly emphasises peer support networks, connecting participants with others who’ve walked similar paths. When you’re sitting in a room with someone who truly gets what it’s like to wake up screaming from a nightmare, or to feel the crushing weight of public expectation, the isolation starts to melt away. It’s a sense of community, a shared understanding that can be profoundly healing. These networks often take the form of veteran-led group therapy sessions, first responder support groups, and sponsor programs. Imagine the relief of finally being able to speak your truth, without judgment, to someone who truly comprehends your struggle. It can be a lifeline.
Family Counseling: Mending the Ripples
Addiction, unfortunately, isn’t a solitary disease; it’s a family disease. Its impact ripples outwards, affecting spouses, children, parents, and close friends. Recognising this deep systemic impact, the program includes crucial family counseling sessions. These sessions aren’t just about ‘fixing’ the person with the addiction; they’re about educating loved ones about the disease, helping them understand its complexities, and providing strategies for rebuilding trust and improving communication. Families learn to set healthy boundaries, to support recovery without enabling, and importantly, they receive their own support for the trauma they’ve endured. For children, particularly, understanding what’s happening and having a safe space to express their feelings can be transformative.
Aftercare Services: Sustaining the Victory
Achieving sobriety is a monumental first step, but sustaining it, that’s the real marathon. So, the program thoughtfully includes robust aftercare services. This isn’t just a handshake and a wish; it’s a comprehensive plan for ongoing support. We’re talking about:
- Follow-up counseling and support groups: Continued therapeutic guidance and peer connection.
- Step-down programs: Gradually reducing the intensity of care as individuals gain stability.
- Outpatient services: Allowing individuals to reintegrate into daily life while still receiving structured support.
- Sober living options: Safe, drug-free environments that provide structure and accountability.
- Vocational training and educational support: Helping individuals find meaningful employment or pursue further education, which is critical for long-term stability and purpose.
- Financial counseling: Addressing often-overlooked practical challenges that can derail recovery.
These services are absolutely crucial for relapse prevention, providing a safety net and a roadmap for navigating the inevitable challenges that life throws at you, even in recovery. Because, let’s be honest, life doesn’t stop just because you’re sober.
A Symphony of Support: The Power of Collaborative Efforts
The sheer scale and complexity of this initiative mean no single entity could possibly go it alone. The success of Florida’s program isn’t just about what the state does; it’s fundamentally about who they’ve brought to the table. It hinges on a delicate, yet powerful, collaboration among a diverse array of stakeholders, each bringing their unique expertise and resources to the fight. It’s a true ecosystem of care, truly.
Government Agencies: The Orchestrators
At the heart of this collaborative effort are various state departments, acting as the primary orchestrators. The Florida Department of Health (DOH) plays a pivotal role, particularly through initiatives like the Helping Emergency Responders Obtain Support (HEROS) Program, which directly targets first responders’ mental health and wellness. Then there’s the Florida Department of Children and Families (DCF), which, under the umbrella of broader initiatives like ‘Hope Florida,’ ensures services are streamlined and accessible, focusing on individual and family well-being. They’ve also been actively enhancing their CORE (Community Outreach and Recovery Effort) program to better serve these populations.
And let’s not forget the Florida Department of Veterans Affairs (FDVA). They are, of course, absolutely central, working tirelessly to connect veterans with the resources they need, whether it’s through the ‘Hope Florida: A Pathway for Patriots’ initiative, which recently celebrated serving its 1,000th veteran, or other outreach efforts. These agencies coordinate information sharing, sometimes establishing joint task forces to tackle specific challenges, and crucially, they allocate funding and develop state-level policies that ensure the program’s reach and sustainability. They’re laying the groundwork, ensuring the legislative and financial backbone is solid.
Healthcare Providers: The Frontline Healers
Next, we have the specialized healthcare providers, the direct caregivers, if you will. Institutions like Rogers Behavioral Health, which has specifically expanded its programs for veterans and first responders into Florida, are absolutely vital. These medical professionals offer truly specialized care, tailored precisely to the complex physiological and psychological needs of these populations. We’re talking about addiction medicine specialists, psychiatrists who understand trauma, therapists trained in military culture, and nurses who provide compassionate, informed care. They’re the ones delivering the evidence-based therapies, administering medication-assisted treatments, and providing the intensive, hands-on support required for complex recovery journeys. They’re developing culturally competent care, understanding that trust isn’t automatically given, it’s earned, especially with groups who’ve often experienced institutional mistrust.
Community Organizations: The Boots on the Ground
Finally, we have the indispensable network of community organizations. These are the non-profits, the local veteran’s groups like the VFW and American Legion, the first responder unions, and benevolent societies. They’re often the first point of contact, the ‘boots on the ground’ who understand the local landscape and can provide immediate, accessible support. Their role extends beyond mere referrals; they offer supplementary services that complement the formal treatment program. This might include: providing temporary housing solutions, assisting with employment searches, offering legal aid, or simply creating safe spaces for fellowship and support. They’re the vital bridge between formal healthcare systems and the everyday needs of individuals in recovery, amplifying the program’s reach and effectiveness in ways government agencies alone couldn’t possibly achieve. They bring that local flavour, that immediate connection, which can be invaluable.
The Ripple Effect: Impact and the Horizon Ahead
While this comprehensive program is still in its relatively early stages, the initial feedback and early indicators are overwhelmingly positive. It’s not just anecdotal, either. Participants are reporting tangible improvements across several key metrics.
They speak of significantly improved mental health, describing a lightness they haven’t felt in years, a lessening of anxiety’s grip. Substance use? That’s demonstrably reduced, with many achieving prolonged periods of sobriety. And perhaps most powerfully, there’s a stronger sense of community emerging, a feeling of belonging that combats the isolation so many have endured. We’re also starting to see encouraging signs in other areas too, things like decreased recidivism rates, improved employment stability, and even family reunification, which is just heartwarming to hear about.
Of course, no program, especially one of this scope, is without its hurdles. Funding is always a perennial challenge; sustaining such intensive, tailored care requires significant, ongoing investment. Scalability is another big one; how do you ensure these high-quality services reach every veteran and first responder across a diverse, geographically expansive state like Florida? Reaching individuals in more rural or remote areas can be particularly tricky, as can overcoming the deeply ingrained stigma that still prevents many from seeking help in the first place.
That said, the future outlook for this initiative appears incredibly promising. There are already plans in place to expand services, delving deeper into specialized care for particular sub-groups within the first responder community – perhaps tailored programs specifically for firefighters, or police officers, given their distinct operational stresses. Incorporation of additional support mechanisms, like dedicated peer mentorship programs beyond group settings, or enhanced vocational training tracks, is also on the drawing board. Imagine what mobile units or expanded telehealth services could do for accessibility, truly bringing the care directly to those who need it, no matter where they are. The vision, certainly, is a robust, sustainable, and truly accessible system of care that leaves no one behind.
A Commitment Honored
Florida’s unwavering commitment to supporting its veterans and first responders through this dedicated addiction recovery program marks an absolutely pivotal step forward. It isn’t just about providing treatment; it’s about acknowledging the profound sacrifices these individuals make every single day for our communities. By offering specialized, comprehensive, and compassionate care, this initiative isn’t just aiding in their recovery; it’s actively honouring their service, restoring their dignity, and helping them rebuild lives of purpose and peace. It’s the least we can do, really, for those who protect us, isn’t it?
Because, at the end of the day, a healthy, supported veteran or first responder strengthens not only their own family but the very fabric of our society. This program is more than just a resource; it’s a profound statement: we see you, we value you, and we’re here for you. And that, my friends, is something truly worth celebrating.
References
-
Florida Department of Health. (n.d.). Helping Emergency Responders Obtain Support (HEROS) Program. Retrieved from (floridahealth.gov)
-
Florida Department of Children and Families. (2025, March 3). Secretary Harris Announces Enhancements to CORE. Retrieved from (myflfamilies.com)
-
Rogers Behavioral Health. (2025, February 18). Rogers’ Program for Veterans, First Responders Now Available in Florida. Retrieved from (rogersbh.org)
-
Florida Department of Veterans’ Affairs. (2025, March 26). Hope Florida: A Pathway for Patriots Reaches 1,000 Veterans Served Milestone. Retrieved from (floridavets.org)
-
Integrated Healthcare Systems. (n.d.). Veterans & First Responders Treatment Program. Retrieved from (integratedhcs.org)


Be the first to comment