Summary
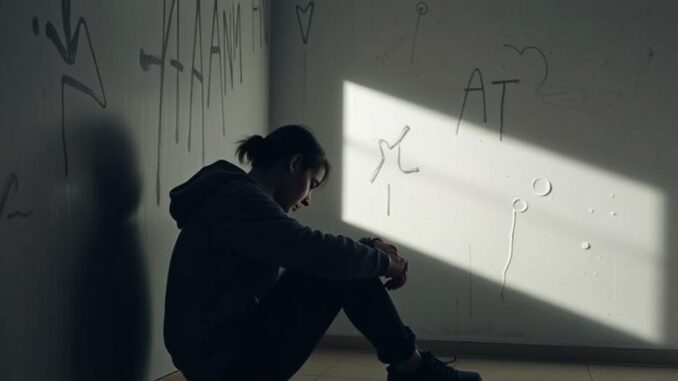
This article explores the link between childhood trauma and increased substance use in adolescents, as well as its unexpected effects on heart rate and blood pressure. It delves into the complexities of this relationship and suggests potential interventions. This article also discusses programs and resources available for recovering addicts.
** Main Story**
Alright, let’s talk about something a little heavy but incredibly important: the impact of childhood trauma on adolescent health. It’s a topic we can’t afford to ignore, especially given its far-reaching consequences. Childhood trauma, experiences like abuse, domestic violence, or the sudden loss of a parent, can leave an indelible mark. The effects? Devastating. It doesn’t just impact a young person’s mental state; it messes with their physical well-being too.
Trauma and Substance Use: A Worrying Connection
You see, there’s this really strong connection between childhood trauma and a higher risk of substance abuse during adolescence. Studies are showing that kids who’ve gone through traumatic experiences are, get this, three times more likely to misuse substances compared to their peers. That’s a staggering number, isn’t it?
And it makes sense, in a heartbreaking way. When someone’s dealing with that level of pain, they might turn to substances to self-medicate, even if it’s a bad idea, or escape from their trauma-related symptoms. Plus, if there’s parental substance misuse in the picture, it’s like throwing fuel on the fire. It’s a double whammy, what with kids, they could have easier access and all.
I remember volunteering at a youth center a few years back, and there was this one kid, Mark. He’d been through so much, it was unbelievable. He started experimenting with drugs early on, and it was clear it was his way of coping with everything that had happened to him. It’s not a conscious choice; it’s a desperate attempt to find some relief.
An Unexpected Twist: Cardiovascular Effects
Now, here’s a curveball. You’d think that childhood trauma would lead to higher heart rates and blood pressure in adolescents, right? That’s what researchers initially thought, too. But guess what? Some studies are finding the opposite. Adolescents who’ve been through more trauma are showing lower heart rates and blood pressure. How weird is that, I thought!
It kind of flies in the face of what we know about childhood trauma and the increased risk of cardiovascular disease later in life. One theory is that it’s linked to certain mental health conditions that sometimes go hand-in-hand with childhood trauma, like conduct disorder. Apparently, conditions like that often come with lower resting heart rates, which might explain the lower cardiovascular readings in these adolescents. More research is needed and, it will likely be complex I would imagine.
So, What Can We Do? Interventions and Recovery
So, where do we go from here? It’s clear that we need to tackle this complex issue head-on. Early intervention programs are essential, focusing on trauma-informed care, teaching kids coping skills, and providing mental health support. I think that they’re really important, don’t you? These programs can help kids process their trauma, build resilience, and find healthier ways to cope, making them less likely to turn to substances.
Resources for Recovery
Thankfully, there are tons of resources available for people struggling with addiction. These include:
- Inpatient and Outpatient Treatment Programs: Offering different levels of support based on individual needs.
- Medication-Assisted Treatment (MAT): Combining medication with therapy for opioid and alcohol dependence. I hear that it is getting much more effective.
- Support Groups: Like AA and NA, providing peer support and a sense of community.
- Family Therapy: Because family involvement is key to recovery.
- Online Resources: Offering virtual support and connections to local resources.
Listen, if you or someone you know is struggling with addiction, please, please reach out for help. There are people who care and resources available. Call local services, health care providers or the SAMHSA’s National Helpline (1-800-662-HELP (4357)). I know it’s hard but it’s a step toward real recovery and things do get better. Remember, recovery is possible with the right support. We all get by with a little help from our friends.
This information is current as of June 3, 2025. Research in this area is constantly evolving, so stay updated on the latest findings.


Be the first to comment