The Evolving Landscape of Addiction Recovery: A New Era of Hope and Healing
You’ve probably noticed it, haven’t you? The conversation around addiction, once whispered in hushed tones, has finally burst into the mainstream. It’s a seismic shift, really, and it’s reflected directly in the unprecedented growth of addiction recovery centers across the United States. We’re witnessing a dramatic expansion, fueled by a surging demand for comprehensive treatment services, and frankly, it’s about time. This isn’t just about more beds; it’s about a fundamental re-evaluation of how we approach addiction, acknowledging its multifaceted nature and the deep complexities involved.
Remember when finding a good center felt like searching for a needle in a haystack, especially one that wasn’t just a revolving door? Well, those days are fading. Especially in places like California, high-tech residential treatment centers are truly setting new benchmarks. They’re not just offering traditional therapy anymore, no, they’re integrating advanced technologies like smart wearables and real-time health monitoring systems, pulling back the curtain on the physiological underpinnings of recovery in a way we’ve never seen before. It’s pretty revolutionary, if you ask me.
The Technological Revolution in Recovery
It’s impossible to discuss modern addiction treatment without talking about technology. We’re living in a digital age, after all, and healthcare, particularly mental health and addiction services, is finally catching up. It’s not just a fancy add-on either, it’s becoming integral to how centers operate and how individuals find lasting sobriety.
Smart Wearables and Real-time Monitoring
Imagine this: you’re in recovery, and your treatment team has insights into your sleep patterns, heart rate variability, even your stress levels, all in real-time. That’s precisely what smart wearables are bringing to the table. These devices, often looking like standard fitness trackers, collect a wealth of biometric data. This isn’t about surveillance, mind you, it’s about creating a personalized, data-driven path to wellness.
For instance, unusual sleep disturbances could flag a potential increase in anxiety or cravings, prompting an early intervention from a therapist. Heart rate spikes that aren’t tied to physical activity? Maybe it’s a trigger response, allowing staff to offer immediate support or adjust therapeutic approaches. They can even send gentle reminders for medication adherence, ensuring individuals stay on track with their prescribed regimens. It’s like having a silent, ever-present coach, providing crucial insights that help individuals and their care teams make more informed decisions. Can you imagine the peace of mind knowing your care team is getting these subtle cues, long before a crisis even begins to brew? It’s genuinely transformative, and it prevents those moments when someone might feel alone and isolated, which can be so detrimental in early recovery.
Telehealth Services and Digital Integration: Bridging Distances
The COVID-19 pandemic, for all its challenges, accelerated one undeniable trend: the widespread adoption of telehealth. For addiction treatment, this wasn’t just a convenience; it was a lifeline. Telemedicine now allows patients to access treatment remotely, smashing through barriers like geographical distance and the limited availability of specialized care, especially in rural areas. Think about someone living hundreds of miles from the nearest qualified addiction specialist. Now, they can connect via a secure video call, receiving the same quality of therapy, counseling, and even medication management. It’s truly leveling the playing field.
But here’s the kicker though, it’s not just about one-on-one video sessions. Digital therapeutics (DTx) are emerging as powerful tools, providing continuous monitoring, personalized feedback, and virtual counseling through mobile apps and online support platforms. These aren’t just feel-good apps; many are FDA-approved, evidence-based programs that deliver cognitive behavioral therapy (CBT) modules, mindfulness exercises, and relapse prevention strategies right to your smartphone. One app might guide you through a meditation session to manage cravings, another might track your mood and offer journaling prompts. These technological advancements are dramatically expanding the reach of addiction treatment services, making them more accessible, more flexible, and ultimately, more effective for a broader population.
Artificial Intelligence and Virtual Reality: The Next Frontier
Looking ahead, artificial intelligence (AI) and virtual reality (VR) hold immense promise for the recovery landscape. AI algorithms can analyze vast amounts of data to predict relapse risks with greater accuracy, allowing for proactive interventions. Imagine an AI identifying patterns in an individual’s digital footprint or biometric data that signal an elevated risk, prompting their care team to reach out before a relapse occurs. AI can also personalize treatment plans, suggesting the most effective therapies based on an individual’s unique profile, something we’re only just beginning to scratch the surface of.
Then there’s VR. It’s not just for gaming anymore. In therapy, VR can create immersive, safe environments for exposure therapy, helping individuals confront triggers in a controlled setting without real-world consequences. A person struggling with alcohol could virtually navigate a bar scene, practicing coping mechanisms in a simulated environment. Or, VR can transport individuals to calming natural landscapes for therapeutic relaxation and mindfulness exercises, enhancing emotional regulation skills. It’s like a training ground for real life, preparing individuals for the challenges they’ll face outside the structured environment of a treatment center.
Innovative Therapies and Holistic Approaches: Nurturing the Whole Person
While technology provides the framework, the heart of recovery lies in healing the person, not just the addiction. This is where the integration of holistic therapies truly shines, gaining significant popularity within the rehabilitation field. These aren’t fads; they’re deeply rooted approaches that aim to address the emotional, spiritual, and physical aspects of addiction recovery, providing a far more comprehensive and sustainable treatment experience.
Beyond the Couch: Diverse Therapeutic Modalities
It’s not just about talk therapy anymore, though that remains a cornerstone. Mindfulness techniques, for instance, teach individuals to stay present, observe thoughts without judgment, and manage cravings or emotional distress. You’d be surprised how empowering simply acknowledging a thought, rather than being consumed by it, can be. Similarly, yoga and other movement therapies help reconnect mind and body, releasing stored tension and promoting self-awareness. It’s a powerful way to reclaim your physical space and reduce stress.
Art therapy, a profoundly non-verbal approach, allows clients to express their emotions and experiences through creative outlets. For someone struggling to articulate deep-seated trauma or shame, a brushstroke or a clay sculpture can communicate volumes. I recall a story from a center in New York where a young man, initially resistant to therapy, found profound healing through painting. He couldn’t voice the pain of his past, but his canvases became a vivid narrative of his journey, a way for his therapists to understand and support him. Similarly, music therapy, engaging clients through listening, singing, or playing instruments, taps into the emotional core, helping process feelings and build self-expression.
And then there’s equine-assisted therapy. Spending time with horses, these majestic, sensitive creatures, teaches individuals about trust, boundaries, communication, and emotional regulation. Horses are incredibly intuitive; they mirror human emotions, providing immediate, honest feedback. It’s an often humbling, yet incredibly rewarding, experience that builds empathy and self-confidence. You learn a lot about yourself when you’re trying to communicate with a 1,000-pound animal!
Beyond these, many centers are now incorporating adventure therapy or wilderness programs, using challenging outdoor activities to build resilience, teamwork, and problem-solving skills. Nutritional counseling is also gaining traction, recognizing the vital link between physical health, brain chemistry, and mental well-being. A healthy gut often means a healthier mind, and in recovery, every advantage counts.
The Expanding Continuum of Care
The days of a one-size-fits-all, 28-day program are largely behind us. Modern addiction treatment understands that recovery is a journey, not a destination, and it requires a spectrum of support. To meet the evolving, often complex needs of clients, centers are diversifying their service offerings, creating a true continuum of care that adapts as an individual progresses.
Evidence-Based Treatment: The Gold Standard
At the core, you’ll find a strong emphasis on evidence-based treatments. Cognitive-behavioral therapy (CBT), for example, helps individuals identify and change problematic thought patterns and behaviors that contribute to addiction. Dialectical behavior therapy (DBT), a highly effective approach for emotional regulation and distress tolerance, is particularly vital for those struggling with co-occurring mental health disorders or intense emotional swings.
Medication-assisted treatment (MAT) is another critical component, rightfully gaining widespread acceptance. Far from ‘trading one addiction for another,’ MAT, utilizing medications like buprenorphine, naltrexone, and methadone, reduces cravings and withdrawal symptoms, giving individuals the stability needed to engage fully in therapy. It’s not a standalone solution, but it’s an incredibly powerful tool when combined with counseling and behavioral therapies. And let’s not forget harm reduction strategies, which prioritize reducing the negative consequences associated with substance use, meeting individuals where they are and promoting incremental, positive change.
Integrated Care Models: Addressing the Whole Picture
One of the most significant shifts is the growing recognition of integrated care models that address both mental health and substance abuse issues simultaneously. It’s a simple truth, yet one often overlooked in the past: addiction rarely travels alone. Co-occurring mental health disorders, like depression, anxiety, or trauma, are incredibly common. Treating one without the other is like trying to fix half a bridge; it just won’t hold.
Treatment centers are increasingly adopting these comprehensive approaches, ensuring that individuals receive care for both their addiction and any underlying mental health conditions. This means therapists specializing in trauma work alongside addiction counselors, and psychiatrists manage medication for both mental health and addiction. It’s about providing truly holistic care that sees the person as a whole, rather than just a diagnosis. This personalized approach, often guided by detailed clinical guidelines, ensures the effectiveness and quality of care, leading to better outcomes and, ultimately, sustained recovery.
Aftercare and Alumni Programs: Sustaining Sobriety
Treatment doesn’t end when someone leaves residential care. In fact, that’s often when the real work begins. Progressive centers are building robust aftercare and alumni programs, recognizing that long-term recovery requires ongoing support. This might include:
- Outpatient Programs: Stepping down from intensive care to less frequent therapy sessions.
- Sober Living Environments: Structured housing that provides a safe, supportive transition back into independent living.
- Peer Support Groups: Connecting individuals with others who understand their journey, fostering a sense of community and shared purpose.
- Alumni Networks: Offering ongoing connection, mentorship opportunities, and social events, reinforcing the message that no one has to walk this path alone.
These ongoing connections are vital. I’ve heard countless stories from individuals who say their alumni network was the backbone of their continued sobriety, a constant reminder that they’re part of something bigger, a community that truly ‘gets it.’
Government Initiatives and Funding: A Public Health Priority
None of this expansion, none of these innovations, would be possible without supportive government initiatives and crucial funding. The federal and state governments have finally, and thankfully, recognized the urgent need to address the addiction crisis, particularly in the wake of the devastating opioid epidemic. They’ve implemented various policies and programs to support treatment efforts, acknowledging that this isn’t just a personal failing, but a public health emergency.
Agencies like the Substance Abuse and Mental Health Services Administration (SAMHSA) and the National Institute on Drug Abuse (NIDA) play pivotal roles. SAMHSA, for instance, provides substantial funding through grants like the State Opioid Response (SOR) grants, which have poured billions into states to expand access to MAT, enhance prevention efforts, and improve overdose reversal services. NIDA, on the other hand, drives the research, ensuring that treatment approaches are grounded in scientific evidence, constantly evolving and improving.
Beyond funding, legislative changes have been instrumental. The Affordable Care Act, with its mental health and substance use disorder parity provisions, mandates that insurance plans cover these services at the same level as medical and surgical care. This has been a game-changer, significantly reducing the financial burden on individuals seeking help. The 21st Century CURES Act also provided critical funding for the opioid crisis, further accelerating the expansion of services. While challenges remain, especially concerning sustained funding and regulatory hurdles, the commitment from government bodies is undeniably a driving force behind the current surge in treatment accessibility and quality.
The Road Ahead: Challenges and Continuing Evolution
Despite the remarkable progress, the journey isn’t without its bumps in the road. We’re still facing significant challenges that require ongoing attention and innovation.
Workforce Shortages
One of the most pressing issues is the shortage of qualified addiction professionals. The demand for therapists, counselors, medical staff, and peer recovery specialists far outstrips the supply. We need more training programs, better compensation, and initiatives to attract talent to this critical field. Without enough skilled hands, even the most innovative centers will struggle to meet the growing need.
Affordability and Accessibility
While insurance parity has helped, affordability remains a major barrier for many. High deductibles, limited in-network providers, and the sheer cost of long-term care can still place treatment out of reach for a significant portion of the population. We also need to consider the ‘digital divide’ – while telehealth is incredible, not everyone has reliable internet access or the necessary devices, creating new forms of inequity.
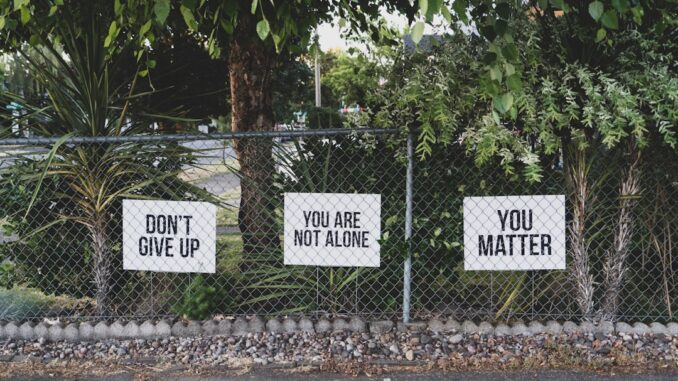
The Persistent Stain of Stigma
And let’s be honest, stigma, that insidious, pervasive barrier, still casts a long shadow. Despite increased public awareness, many individuals still fear judgment, discrimination, or career repercussions if they seek help. This fear often prevents people from reaching out until their addiction has spiraled dangerously. We need to keep pushing the conversation, humanizing addiction, and reframing it as a treatable health condition, not a moral failing. It’s a marathon, not a sprint, this battle against societal prejudice.
Addressing Relapse: A Reality, Not a Failure
Finally, we must continually refine our understanding and approach to relapse. It’s a natural, often expected, part of the recovery process for many, not a sign of failure. Centers are increasingly integrating robust relapse prevention planning and embracing harm reduction principles as part of the overall strategy. The goal isn’t just to get someone sober, but to equip them with the tools and resilience to navigate the inevitable challenges of life without resorting to substances.
In Conclusion
So, what does all this mean for the future of addiction recovery? It’s a story of transformation, wouldn’t you say? The expansion of addiction recovery centers is a direct, vibrant response to a growing, undeniable demand for comprehensive and truly innovative treatment services. By embracing technological advancements, by deeply integrating holistic therapies, and by committing to personalized, integrated care models, these centers aren’t just treating symptoms; they’re healing individuals, addressing the ghosts of past choices and building solid foundations for future wellness.
This isn’t just an evolution; it’s a revolution in how we approach addiction treatment. It emphasizes accessibility, celebrates effectiveness, and champions individualized care, weaving a rich tapestry of interconnected support. It’s messy, it’s challenging, but it’s filled with a renewed sense of hope, and honestly, that’s something we can all get behind. The future of recovery looks brighter, more inclusive, and significantly more intelligent than ever before.
References


Be the first to comment