The Strategic Allocation of Opioid Settlement Funds in Colorado: A Comprehensive Analysis of Public Health Infrastructure Investments
Many thanks to our sponsor Maggie who helped us prepare this research report.
Abstract
The opioid crisis represents an unprecedented public health catastrophe, compelling states across the United States to devise and implement multifaceted strategies to mitigate its devastating consequences. Colorado, at the forefront of this national response, has successfully secured substantial settlements from pharmaceutical entities and distributors whose practices significantly contributed to the epidemic’s proliferation. This exhaustive report undertakes a detailed examination of Colorado’s strategic and judicious allocation of these monumental funds. The analysis focuses on pivotal investments across critical domains, including the establishment and expansion of sophisticated treatment facilities, the development of supportive sober living housing, the deployment of innovative mobile harm reduction units, and the foundational support for recovery-focused educational institutions, with a particular emphasis on addressing disparities in historically underserved and geographically remote regions. By meticulously scrutinizing the theoretical underpinnings, practical implementation, observed effectiveness, inherent challenges, and long-term sustainability considerations of these initiatives, this report aims to provide a comprehensive assessment of their collective potential to fundamentally reshape the addiction recovery landscape within Colorado and offer transferable insights for other affected jurisdictions.
Many thanks to our sponsor Maggie who helped us prepare this research report.
1. Introduction
The opioid epidemic has cast a long and shadow over communities throughout the United States, manifesting as a severe public health, social, and economic crisis. Colorado, mirroring the national trajectory, has grappled with the pervasive and escalating impacts of opioid use disorder (OUD), including a significant surge in overdose fatalities, increased strain on healthcare systems, and profound disruptions to societal fabric. In a landmark response to this enduring crisis, the State of Colorado has been a key beneficiary of substantial financial settlements resulting from extensive litigation against pharmaceutical manufacturers and distributors deemed culpable for their roles in fueling the epidemic through deceptive marketing practices and inadequate oversight of drug distribution. These considerable funds, collectively amounting to hundreds of millions of dollars over multiple years, represent an unparalleled opportunity—and a profound responsibility—for Colorado to implement a holistic, evidence-based, and sustainable framework designed not merely to abate the current crisis but to fortify the state’s public health infrastructure against future iterations of substance use disorders. This report embarks on an in-depth exploration of Colorado’s meticulous utilization of these settlement funds, critically evaluating the transformative impact of strategic investments across four primary pillars: enhanced treatment infrastructure, robust supportive housing solutions, dynamic harm reduction interventions, and specialized educational initiatives tailored for individuals in recovery. Through this comprehensive analysis, we aim to shed light on Colorado’s pioneering approach to addiction recovery, identifying both its successes and the persistent challenges that underscore the complexity of public health remediation efforts on such a grand scale.
Many thanks to our sponsor Maggie who helped us prepare this research report.
2. Background
2.1 The Opioid Crisis in Colorado: A Longitudinal Perspective
Colorado’s experience with the opioid crisis, while aligning with national trends, presents distinct characteristics shaped by its unique demographics, geography, and socio-economic landscape. The crisis in Colorado, much like the broader national narrative, unfolded in successive waves. The initial wave, beginning in the late 1990s, was primarily driven by the over-prescription of opioid painkillers, fueled by aggressive marketing campaigns that downplayed addiction risks and promoted opioids for chronic pain management. Colorado, with its significant rural populations and prevalent work in physically demanding industries (e.g., agriculture, mining, construction), saw a widespread adoption of these prescriptions, leading to a surge in OUD diagnoses. By the mid-2000s, as prescribing practices tightened, many individuals who had become dependent on prescription opioids transitioned to more readily available and often cheaper illicit alternatives, marking the second wave, characterized by a rise in heroin use. The most recent and deadly wave, commencing in the 2010s and accelerating rapidly, has been dominated by the proliferation of highly potent synthetic opioids, particularly fentanyl. Fentanyl, often illicitly manufactured and frequently mixed into other drugs (e.g., heroin, cocaine, counterfeit pills) without the user’s knowledge, has dramatically increased overdose fatality rates due to its extreme potency and unpredictability. Colorado has witnessed a significant increase in fentanyl-related deaths, posing an immense challenge for emergency services and public health officials.
Statistical data from the Colorado Department of Public Health and Environment (CDPHE) indicates a distressing trend. While there was a slight dip in opioid overdose deaths in the mid-2010s, likely due to initial efforts to curb prescription opioid access, the advent of fentanyl reversed this progress, leading to record high overdose fatalities in recent years. For instance, preliminary data for 2021 indicated over 1,800 drug overdose deaths in Colorado, with opioids, particularly fentanyl, being a primary contributor. The crisis has disproportionately affected certain demographics, including young adults, individuals experiencing homelessness, and specific racial and ethnic minority groups. Furthermore, the state’s diverse geography presents unique challenges; rural areas often suffer from limited access to healthcare infrastructure, including addiction treatment specialists, while urban centers face high concentrations of individuals experiencing homelessness and poverty, exacerbating vulnerability to OUD. The economic toll on the state has been profound, encompassing increased healthcare expenditures, lost productivity, strained criminal justice resources, and significant social costs borne by families and communities.
2.2 Legal Framework of Opioid Settlements: Genesis and Structure
The substantial financial settlements now benefiting Colorado are the culmination of a multi-year, multi-state legal offensive against the pharmaceutical industry. The genesis of these legal actions lies in the assertion by states, counties, and municipalities that opioid manufacturers engaged in deceptive marketing practices, downplaying the addictive nature of their products, while distributors failed to adequately monitor and report suspicious orders, thus flooding communities with opioid pills. Key defendants in these litigations included major manufacturers like Purdue Pharma (maker of OxyContin), Johnson & Johnson (producer of opioid ingredients and products), and distributors such as McKesson, AmerisourceBergen, and Cardinal Health. The legal arguments frequently centered on public nuisance claims, alleging that these companies’ actions created a public health crisis that necessitated immense public expenditure for remediation.
These protracted legal battles ultimately led to a series of nationwide settlement agreements, the largest of which are the Manufacturer and Distributor Settlements, totaling over $50 billion nationally. Colorado’s participation in these agreements entitles the state to a significant portion of these funds, earmarked exclusively for opioid abatement activities. The terms of these settlements are highly structured, dictating how the funds must be allocated to ensure they directly address the opioid crisis. A crucial element of the Colorado framework is the establishment of the Colorado Opioid Abatement Council (COAC). This council, comprising representatives from various state agencies, local governments, and community stakeholders, is tasked with overseeing the equitable and effective distribution of Colorado’s share of the settlement funds. The COAC’s mandate, as stipulated in state legislation and the settlement agreements, is to ensure that investments align with evidence-based strategies for prevention, treatment, harm reduction, and recovery support. The funds are typically distributed across state-level initiatives and local government allocations, fostering both statewide strategic coherence and localized responsiveness to community-specific needs. This intricate legal and administrative framework underscores a collective commitment to transform the resources gained from accountability into tangible improvements in public health.
Many thanks to our sponsor Maggie who helped us prepare this research report.
3. Allocation of Opioid Settlement Funds in Colorado
Colorado’s strategic allocation of opioid settlement funds is guided by a comprehensive public health framework designed to address the crisis across multiple intervention points. The Colorado Opioid Abatement Council (COAC) plays a central role in prioritizing and disbursing these funds, ensuring alignment with evidence-based practices and a focus on underserved populations. The investments span a critical continuum of care, from immediate life-saving interventions to long-term recovery support.
3.1 Treatment Facilities: Expanding Access and Enhancing Quality
Recognizing that robust treatment infrastructure is foundational to combating OUD, Colorado has made significant investments in the establishment, expansion, and enhancement of treatment facilities. This multi-pronged approach aims to ensure a comprehensive continuum of care, addressing the diverse and evolving needs of individuals seeking recovery. Funds have been directed towards a variety of treatment modalities, including:
- Inpatient Residential Treatment: Supporting facilities that provide 24/7 structured care, often including medical detoxification, individual and group therapy, life skills training, and integrated mental health services. The focus is on increasing bed capacity and improving the quality of therapeutic environments.
- Intensive Outpatient Programs (IOP) and Outpatient Programs (OP): Expanding access to less restrictive but still highly structured treatment options that allow individuals to maintain employment or family responsibilities while receiving regular therapy, counseling, and medication-assisted treatment (MAT) support. Funds support staffing, facility upgrades, and the integration of telehealth services to improve accessibility.
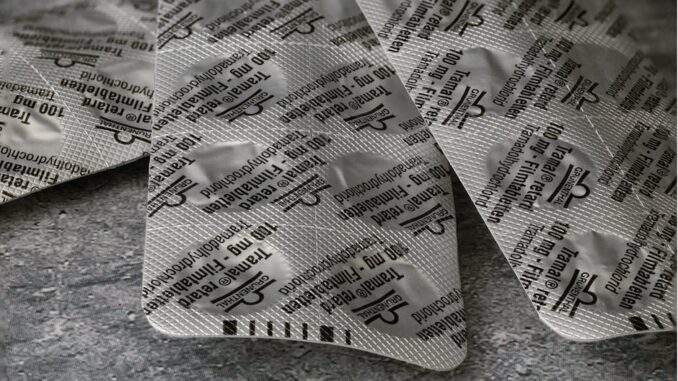
- Medication-Assisted Treatment (MAT) Clinics: MAT, combining behavioral therapies with medications like buprenorphine, naltrexone, and methadone, is considered the gold standard for OUD treatment. Funds are used to establish new MAT clinics, expand existing ones, train more healthcare providers (physicians, nurse practitioners, physician assistants) to prescribe MAT, and reduce barriers to access, particularly in rural areas where MAT providers are scarce.
- Withdrawal Management (Detoxification) Centers: Supporting safe and medically supervised withdrawal processes, which are often the critical first step in recovery. Funds help increase bed capacity and ensure these centers are equipped with trained medical staff and appropriate protocols.
In a notable example of this strategic investment, the Colorado Opioid Abatement Council awarded $5 million in May 2023 to 12 organizations and local governments across the state specifically for ‘opioid infrastructure funding’ (Colorado Attorney General, 2025). This funding directly supports capital improvements and operational necessities for recovery services. Examples include:
- Increased Bed Capacity: Funding enabled several facilities to add new beds for residential treatment or withdrawal management, significantly reducing waitlists that often deter individuals from seeking help during critical moments.
- Facility Renovations and Upgrades: Improving existing treatment environments to create more therapeutic, safe, and welcoming spaces, sometimes incorporating trauma-informed design principles.
- Technology Integration: Investments in telehealth infrastructure allow for remote access to therapy, counseling, and MAT follow-ups, particularly beneficial for individuals in rural or underserved areas who face transportation barriers.
- Workforce Development: Supporting training programs for addiction counselors, peer recovery coaches, and medical staff, addressing the persistent workforce shortages in the behavioral health sector.
- Integrated Care Models: Funds facilitated the development of programs that integrate OUD treatment with primary healthcare and mental health services, recognizing the high prevalence of co-occurring disorders. For instance, a facility might use funds to hire a mental health therapist or a primary care nurse to provide on-site services, streamlining patient care.
The strategic intent behind these investments is to create a robust, accessible, and high-quality treatment ecosystem that can effectively respond to the scale and complexity of the opioid crisis. The COAC’s criteria for funding emphasize evidence-based practices, geographic equity, and sustainability, aiming for long-term impact beyond the initial funding period.
3.2 Sober Living Housing: Fostering Sustainable Recovery Environments
Recognizing that stable and supportive housing is a critical determinant of long-term recovery success, Colorado has allocated substantial settlement funds to develop and expand sober living environments. These residences serve as crucial transitional spaces, bridging the gap between intensive treatment and full reintegration into independent living. The rationale for investing in sober living is rooted in extensive research demonstrating that individuals residing in supportive recovery housing experience lower rates of relapse, increased employment, and improved overall well-being compared to those without such support.
Colorado’s investments support various models of sober living, predominantly focusing on facilities that adhere to established standards, often guided by organizations such as the National Alliance for Recovery Residences (NARR). Key aspects of these investments include:
- Property Acquisition and Renovation: Funds are used to purchase properties or renovate existing ones to create safe, structured, and recovery-oriented living spaces. This includes ensuring compliance with health, safety, and zoning regulations.
- Operational Support and Staffing: Providing financial assistance for the operational costs of these residences, including utilities, maintenance, and the salaries of house managers or peer support specialists who often live on-site or provide regular supervision.
- Integrated Support Services: Critically, these residences are not merely housing but are designed to offer a comprehensive suite of support services. As noted by the Colorado Attorney General, the Colorado Opioid Abatement Council’s funding explicitly supports recovery residences that provide access to medication-assisted treatment (MAT) and on-site peer support (Colorado Attorney General, 2024). This integration means residents receive:
- MAT Access: Facilitated connections to MAT providers, ensuring continuity of medication if needed.
- Peer Support: The presence of certified peer recovery coaches, often individuals with lived experience in recovery, who provide mentorship, empathy, and practical guidance, fostering a strong sense of community and accountability.
- Life Skills Training: Workshops on budgeting, job searching, healthy cooking, and conflict resolution.
- Referral Services: Connections to vocational training, educational opportunities, mental health services, and legal aid.
- Structured Environment: Implementation of house rules, regular meetings, and expectations for participation in recovery-oriented activities (e.g., 12-step programs, group therapy).
The strategic goal is to create environments where individuals can strengthen their sobriety, develop essential life skills, and build supportive networks, all while navigating the complexities of post-treatment life. By reducing the stress associated with homelessness or unstable living situations, sober living housing significantly enhances the likelihood of sustained recovery. Challenges remain in scaling these initiatives to meet the immense demand, as well as addressing ‘Not In My Backyard’ (NIMBY) sentiments from communities, and ensuring consistent quality and oversight across all funded residences.
3.3 Mobile Harm Reduction Units: Reaching Underserved Populations
Colorado’s investment in mobile harm reduction units represents a pragmatic and compassionate approach to addressing the immediate and life-threatening consequences of opioid use, particularly in hard-to-reach and underserved populations. Harm reduction is a public health philosophy and set of interventions aimed at reducing the negative consequences associated with drug use, without necessarily requiring abstinence as a prerequisite. It acknowledges the realities of drug use and seeks to minimize harm to individuals and communities.
These mobile units are essentially clinics on wheels, equipped to deliver critical services directly to communities where access to traditional healthcare facilities is limited, or where individuals face significant barriers to seeking help due to stigma, lack of transportation, or homelessness. Services typically provided by Colorado’s mobile harm reduction units include:
- Naloxone Distribution and Training: Providing the opioid overdose reversal medication naloxone (Narcan) to individuals who use drugs, their families, and community members, along with comprehensive training on how to recognize and respond to an overdose. This intervention has been proven to significantly reduce overdose fatalities.
- Fentanyl Test Strip Distribution: Offering test strips that allow individuals to check their drugs for the presence of fentanyl, enabling them to make more informed decisions and reduce their risk of accidental overdose.
- Syringe Service Programs (SSPs): Providing sterile syringes and safe disposal options, which significantly reduce the transmission of blood-borne diseases like HIV and Hepatitis C among people who inject drugs. These programs also offer a vital point of contact for health services.
- Wound Care and Basic Medical Screenings: Addressing common health issues associated with injection drug use, such as skin infections, and offering screenings for STIs and other health conditions.
- Education on Safer Use Practices: Providing non-judgmental information on how to reduce risks associated with drug use, including overdose prevention and vein care.
- Referral to Treatment and Social Services: A crucial function of these units is to serve as an ‘on-ramp’ to broader care. Staff connect individuals with OUD treatment (including MAT), mental health services, housing support, and other social welfare programs. This includes direct referrals and, in some cases, immediate linkage to care.
An exemplary initiative is supported by the Boulder County Regional Opioid Council’s ‘On-ramp to Resilience Project’ (Colorado Attorney General, 2025). While this project supports a new multi-regional treatment facility, the mobile harm reduction units play a vital role in its overall strategy. They act as the initial point of contact, building trust and providing immediate life-saving interventions in the community. Through this engagement, individuals are then guided and supported in accessing the comprehensive, trauma-informed services offered by the central facility, which includes medication-assisted treatment, intensive outpatient programs, withdrawal management, residential programming, and crucial care coordination across multiple systems. This integrated model ensures that immediate harm reduction efforts are seamlessly linked to longer-term recovery pathways, maximizing the impact of the settlement funds by creating a complete loop of support. The challenges for these units include staffing highly skilled and compassionate outreach workers, ensuring the safety of staff in the field, and overcoming community resistance or misunderstanding of harm reduction principles.
3.4 Recovery-Focused Schools: Nurturing Youth in Recovery
Addressing the unique needs of adolescents and young adults affected by the opioid crisis, Colorado has innovatively directed settlement funds towards the establishment and support of recovery-focused schools. Traditional school environments can pose significant challenges for students in recovery from substance use disorders, including exposure to substance-using peers, lack of understanding from staff, and difficulty balancing academic demands with recovery commitments. Recovery high schools offer a tailored solution, integrating academic instruction with comprehensive recovery support services.
These specialized educational institutions are designed to provide a safe, sober, and academically rigorous environment that prioritizes both educational attainment and sustained recovery. The model typically includes:
- Integrated Academic and Recovery Support: Students receive a full academic curriculum leading to a high school diploma, alongside a robust system of recovery support. This includes individual and group counseling, peer support meetings, life skills development, and relapse prevention strategies.
- Qualified Staff: Teachers and administrators are often trained in addiction science, trauma-informed care, and adolescent development, creating an understanding and empathetic learning environment.
- Peer Community: A crucial component is the development of a strong peer community. Students are surrounded by others who are also committed to sobriety, fostering mutual support, accountability, and a sense of belonging that combats the isolation often experienced by young people in recovery.
- Family Engagement: Recovery schools often involve families in the recovery process, offering support, education, and family counseling to create a supportive home environment.
- Post-Secondary Pathways: Beyond academics, these schools focus on preparing students for successful futures, including college matriculation, vocational training, and meaningful career pathways, as highlighted by the Colorado Attorney General (Colorado Attorney General, 2025).
Colorado’s commitment to this model is exemplified by the Colorado Charter School Institute’s (CSI) statewide recovery high school network, which has received significant funding from the Colorado Opioid Abatement Council. This network includes the establishment of two new recovery high schools in Aurora and Colorado Springs. These schools are designed to offer a unique educational experience where academic excellence is pursued within a supportive culture of recovery. They aim to reduce relapse rates among young people, improve their academic outcomes, and equip them with the skills and confidence necessary for long-term well-being and productive citizenship. The challenges for recovery schools include scalability due to the specialized nature of their services, securing sustainable long-term funding beyond the initial settlement funds, and the need for highly specialized staff who can effectively manage both academic and recovery support components.
Many thanks to our sponsor Maggie who helped us prepare this research report.
4. Impact Assessment
Evaluating the true impact of Colorado’s opioid settlement fund allocation requires a multi-dimensional assessment that considers both quantitative metrics and qualitative improvements in the lives of individuals and communities. While comprehensive long-term data collection is ongoing, early indicators and theoretical frameworks suggest significant positive developments, alongside persistent challenges.
4.1 Treatment Facilities: Enhancing Capacity and Outcomes
The expansion and enhancement of treatment facilities funded by the opioid settlements have undeniably bolstered Colorado’s capacity to address OUD. The primary impact has been a quantifiable increase in access to care, particularly in regions that were previously identified as treatment deserts. This expansion translates to shorter wait times for admission, crucial for individuals experiencing acute crises, and a broader availability of diverse treatment modalities, including MAT, which is essential for evidence-based care.
Metrics of Success: Early indicators suggest improvements in key outcome metrics, including:
- Increased Treatment Retention Rates: Studies show that easier access to appropriate treatment, coupled with comprehensive support services, leads to individuals remaining in care for longer durations, which is strongly correlated with improved outcomes.
- Reduced Relapse Rates: While difficult to attribute solely to facility expansion, the availability of comprehensive, integrated care that addresses co-occurring mental health disorders and provides post-treatment support contributes to lower relapse rates.
- Improved Patient Outcomes: This encompasses a range of indicators such as reduced illicit drug use, decreased overdose incidents, improved physical and mental health, increased employment, and reduced involvement with the criminal justice system.
- Geographic Equity: Anecdotal evidence suggests that new facilities or expanded services in rural or historically underserved areas have begun to close critical gaps in access.
Challenges and Limitations: Despite these promising signs, significant challenges persist:
- Workforce Shortages: A critical barrier is the chronic shortage of qualified addiction specialists, including physicians, nurses, therapists, and peer recovery coaches. While funds support training, the pipeline is slow, and competition for skilled professionals is fierce. This impacts the quality of care and the ability to sustain expanded services.
- Complexity of Co-occurring Disorders: A high percentage of individuals with OUD also experience co-occurring mental health disorders (e.g., anxiety, depression, PTSD) and other substance use disorders. Ensuring that facilities are truly equipped to provide integrated, holistic care for these complex presentations remains an ongoing challenge, requiring specialized training and staffing.
- Stigma and Engagement: Despite increased access, stigma surrounding addiction and treatment continues to deter individuals from seeking help. Effective outreach and community education are vital, but hard to measure.
- Data Interoperability: A persistent challenge lies in developing robust, integrated data collection systems across diverse treatment providers to consistently track long-term patient outcomes, treatment pathways, and service gaps. Without this, a comprehensive, real-time assessment of the investment’s full impact is difficult.
- Sustainability Beyond Settlement Funds: While settlement funds provide an initial boost, ensuring the long-term operational sustainability of these expanded facilities beyond the finite period of settlement disbursements requires diversified funding streams, including state appropriations, private insurance reimbursements, and Medicaid expansion.
4.2 Sober Living Housing: Building Foundations for Sustained Recovery
Investments in sober living housing have proven instrumental in providing individuals with a stable, supportive environment crucial for navigating the challenging transition from intensive treatment to sustained community integration. The impact of these residences extends beyond mere shelter, fostering environments conducive to long-term sobriety and personal growth.
Impact Metrics:
- Reduced Relapse Rates: Research consistently demonstrates that individuals who transition into stable sober living environments after treatment exhibit significantly lower rates of relapse compared to those discharged to unstable or unsupportive settings. The structured environment, peer support, and accountability mechanisms are key contributing factors.
- Increased Treatment Retention and Engagement: Sober living often provides a bridge that allows individuals to continue outpatient treatment, attend recovery meetings, and engage with peer support networks, reinforcing their commitment to recovery.
- Improved Life Functioning: Residents often show improvements in employment rates, educational attainment, financial stability, and overall independent living skills. The supportive community within these residences helps residents develop practical skills and build positive social networks.
- Decreased Criminal Justice Involvement: By providing stability and support, sober living can reduce instances of homelessness, illicit drug use, and associated criminal activity, leading to fewer re-arrests and interactions with the justice system.
- Enhanced Social Support: The peer-led model fosters a sense of community and belonging, reducing feelings of isolation and providing a ready support system during challenging times.
Challenges and Limitations: Despite the clear benefits, the sober living initiative faces several hurdles:
- Limited Availability and High Demand: While new residences are being funded, the overall supply of quality sober living housing still falls far short of the demand in Colorado, particularly for specific populations (e.g., individuals with co-occurring mental health disorders, parents with children, justice-involved individuals).
- Quality Control and Oversight: Ensuring that all funded sober living residences adhere to high standards of care, ethical practices, and safety protocols is paramount. While some states have robust certification processes (e.g., NARR affiliation), inconsistent oversight can lead to variable quality and, in some cases, exploitative practices.
- Community Resistance (NIMBYism): Establishing new sober living homes can often encounter significant resistance from local communities and residents due to misconceptions about individuals in recovery, leading to zoning challenges and public opposition.
- Funding Sustainability: Many sober living models rely on a mix of resident fees, grants, and limited public funding. Ensuring long-term financial viability beyond the settlement funds requires exploring diverse and stable funding mechanisms, such as integrating sober living into healthcare reimbursement models.
- Integration with the Continuum of Care: Seamless transitions from acute treatment to sober living, and then to independent living, require strong care coordination and robust referral pathways, which are not always consistently developed.
4.3 Mobile Harm Reduction Units: Expanding Reach and Saving Lives
Mobile harm reduction units have emerged as a highly effective and adaptable strategy to address the immediate and acute consequences of the opioid crisis, particularly for marginalized and hard-to-reach populations. Their flexibility allows for rapid deployment to emerging hotspots and underserved areas, acting as critical points of contact for life-saving interventions.
Impact Metrics:
- Increased Naloxone Distribution and Overdose Reversals: The most immediate and measurable impact is the wide distribution of naloxone, directly empowering individuals and communities to prevent fatal overdoses. Reports indicate a significant number of reported overdose reversals facilitated by distributed kits.
- Engagement with High-Risk Populations: Mobile units successfully reach individuals who are disconnected from traditional healthcare systems, including people experiencing homelessness, those in active addiction, and individuals in rural areas with limited services. This direct engagement fosters trust and opens doors to further interventions.
- Reduced Disease Transmission: Syringe service programs (SSPs) offered via mobile units are instrumental in reducing the incidence of HIV, Hepatitis C, and other blood-borne infections associated with injection drug use, thereby mitigating broader public health threats.
- Facilitated Referrals to Treatment: Beyond immediate harm reduction, these units serve as critical ‘on-ramps’ to treatment, housing, and social services. By building rapport and providing non-judgmental support, staff successfully link individuals to more comprehensive care, as exemplified by the Boulder County ‘On-ramp to Resilience Project.’
- Increased Awareness and Education: Mobile units play a crucial role in public health education, dispelling myths about drug use, promoting safer practices, and building community understanding of harm reduction principles.
Challenges and Limitations: Despite their success, mobile harm reduction units face several operational and systemic challenges:
- Logistical Complexity: Operating mobile units involves significant logistical challenges, including staffing (requiring highly skilled and compassionate outreach workers), vehicle maintenance, secure storage of supplies (e.g., naloxone, syringes), and ensuring staff safety in diverse community settings.
- Community Acceptance and Misconceptions: Harm reduction remains a controversial approach in some communities, often misinterpreted as ‘enabling’ drug use. This can lead to resistance from local residents, law enforcement, or political entities, impacting the ability to operate effectively.
- Funding Volatility: While settlement funds provide a boost, the long-term sustainability of mobile harm reduction services often relies on precarious grant funding or year-to-year state appropriations, making long-term planning and expansion difficult.
- Scope of Services and Follow-Up: While excellent at immediate interventions and referrals, the mobile nature inherently limits the depth of medical or therapeutic services that can be provided on-site, necessitating robust follow-up systems that are sometimes challenging to maintain.
- Data Collection and Privacy: Collecting consistent and comprehensive data on services provided and outcomes achieved, while maintaining client privacy, can be complex in a mobile, outreach-based setting.
4.4 Recovery-Focused Schools: Empowering Youth for Academic and Personal Success
Recovery-focused schools represent a specialized and highly impactful investment, addressing the unique educational and social needs of adolescents and young adults in recovery from substance use disorders. These institutions provide a critical bridge, allowing students to pursue academic success within an environment that explicitly supports their sobriety.
Impact Metrics:
- Improved Academic Outcomes: Students in recovery schools often demonstrate higher attendance rates, improved grades, and increased graduation rates compared to their peers in traditional schools who are also in recovery. The tailored academic support and reduced external pressures contribute significantly to this.
- Reduced Relapse Rates Among Youth: The sober peer environment, integrated recovery support services, and dedicated staff trained in addiction and adolescent development significantly reduce the likelihood of relapse among students.
- Enhanced Social-Emotional Development: These schools foster a strong sense of community and belonging, helping students develop healthy coping mechanisms, communication skills, and positive self-esteem often impacted by their substance use history.
- Pathways to Higher Education and Career: By integrating academic learning with life skills and career exploration, recovery schools effectively prepare students for post-secondary education, vocational training, or direct entry into the workforce, contributing to long-term economic stability and social integration.
- Positive Feedback from Students and Parents: Qualitative data consistently indicates high levels of satisfaction from students who feel understood, safe, and supported, and from parents who express relief and gratitude for a specialized environment that caters to their child’s unique needs.
Challenges and Limitations: Despite their demonstrated efficacy, recovery-focused schools face specific challenges:
- Scalability and Limited Capacity: Given the specialized nature of these schools and the intensive support they provide, their capacity is often limited. While the establishment of new schools in Aurora and Colorado Springs is significant, they can only serve a fraction of the youth population in recovery across the state.
- Specialized Staffing Needs: Attracting and retaining highly qualified staff who possess expertise in both education and addiction/recovery (e.g., certified addiction counselors, teachers with trauma-informed training) is a significant challenge. This specialized workforce often commands higher salaries or requires specific training pipelines.
- Funding Sustainability: As with other initiatives, long-term funding beyond initial settlement funds is crucial. Recovery schools typically require more resources per student than traditional public schools due to the intensive support services offered. Securing consistent state and federal funding streams is vital for their continued operation and expansion.
- Geographic Accessibility: While new schools address needs in specific urban centers, students in remote or rural areas may still face significant barriers to access, including transportation and the need to relocate.
- Referral and Enrollment Processes: Ensuring effective referral pathways from treatment centers, juvenile justice systems, or traditional schools to recovery schools requires coordinated efforts and clear communication among various agencies.
In summary, Colorado’s investments across these four pillars are demonstrably creating positive impacts, particularly in enhancing accessibility to critical services. However, a holistic assessment reveals that the success of these initiatives is intertwined with addressing persistent systemic challenges related to workforce development, funding diversification, community engagement, and the integration of services across the broader public health ecosystem.
Many thanks to our sponsor Maggie who helped us prepare this research report.
5. Challenges and Considerations
While Colorado’s strategic allocation of opioid settlement funds has initiated a commendable transformation of the state’s addiction recovery infrastructure, ensuring the enduring impact and equitable reach of these initiatives necessitates addressing several inherent challenges and critical considerations. These factors determine not only the immediate effectiveness of the programs but also their long-term viability and their capacity to adapt to the evolving landscape of the opioid crisis.
5.1 Sustainability Beyond Settlement Funds
Perhaps the most pressing challenge for all initiatives funded by opioid settlements is long-term sustainability. The settlement funds, while substantial, are finite and often disbursed over many years, creating a potential ‘funding cliff’ once these payments cease. Without proactive planning, programs that prove effective could face severe cuts or closure, undoing much of the progress achieved.
- Diversification of Funding Streams: It is paramount for Colorado to develop and implement strategies for diversifying funding beyond the settlement moneys. This includes advocating for consistent state appropriations in the annual budget process, leveraging federal grants (e.g., SAMHSA, HRSA), exploring opportunities through Medicaid expansion and reimbursement for addiction services, and fostering partnerships with private philanthropy and foundations. Moving towards value-based care models, where providers are reimbursed based on patient outcomes rather than just services rendered, could also incentivize sustainable, effective care.
- Building Self-Sustaining Models: Programs should be designed with an eye towards operational efficiency and cost-effectiveness. This might involve integrating services to reduce overhead, developing robust billing practices for eligible services (e.g., through commercial insurance or Medicaid), and investing in preventative measures that reduce the long-term burden on healthcare and social systems.
- Advocacy and Policy Changes: Sustained political will and legislative action are critical. Advocates must continually demonstrate the return on investment of addiction treatment and recovery services to secure ongoing public funding and supportive policies that prioritize these essential public health interventions.
5.2 Equity and Access for All Communities
Despite efforts to target underserved regions, significant disparities in access to and outcomes from addiction services persist. Ensuring that all communities, especially those historically marginalized, benefit equitably from these investments is a moral imperative and a public health necessity. These disparities are often rooted in systemic inequities related to race, ethnicity, socio-economic status, geographic location, sexual orientation, gender identity, and justice system involvement.
- Targeted Outreach and Engagement: Initiatives must employ targeted outreach strategies to reach populations that have been underserved or are hesitant to access traditional services due to historical mistrust, cultural barriers, or lack of awareness. This involves working with community-based organizations, faith leaders, and trusted local figures.
- Culturally Competent and Linguistically Appropriate Services: Programs must be designed and delivered in a manner that is culturally sensitive and linguistically appropriate for diverse populations. This includes hiring diverse staff, providing training on cultural humility, and offering services in multiple languages to overcome communication barriers.
- Addressing Social Determinants of Health: True equity requires addressing the broader social determinants of health that influence addiction and recovery, such as poverty, housing instability, food insecurity, and lack of employment opportunities. Integrated services that connect individuals to these foundational supports are crucial.
- Data Disaggregation and Monitoring: Robust data collection and analysis, disaggregated by demographic factors, are essential to identify existing disparities, track progress, and adjust strategies to ensure equitable distribution of resources and improved outcomes for all groups.
- Focus on Special Populations: Dedicated attention is needed for specific vulnerable groups, including pregnant and parenting individuals, justice-involved populations, individuals experiencing homelessness, and the LGBTQ+ community, who often face unique barriers and stigma in accessing care.
5.3 Integration into Broader Healthcare and Social Systems
The long-term success and efficacy of Colorado’s opioid abatement initiatives hinge on their seamless integration into the broader healthcare, mental health, and social services systems. Addiction is a chronic disease influenced by biological, psychological, and social factors, requiring a holistic and coordinated approach to care that extends beyond standalone treatment.
- Continuum of Care Coordination: Efforts must focus on creating robust care coordination and navigation services that ensure smooth transitions between different levels of care (e.g., detoxification to residential treatment, residential to sober living, sober living to outpatient care). This requires interoperable data systems and shared protocols among providers.
- Interagency Collaboration: Collaborative efforts among various state agencies (e.g., Health, Human Services, Public Safety, Education), local governments, and community-based organizations are critical. This facilitates a ‘no wrong door’ approach where individuals can access support regardless of where they first seek help.
- Primary Care Integration: Integrating OUD screening, brief intervention, and referral to treatment (SBIRT) into primary care settings is vital for early identification and intervention. Training primary care providers to offer MAT further expands access to essential medication.
- Linkages with Criminal Justice and Child Welfare Systems: A significant portion of individuals with OUD interact with the criminal justice and child welfare systems. Developing strong partnerships with these sectors can facilitate diversion programs, provide treatment within correctional settings, and support family reunification.
- Whole-Person Care: Recognizing that addiction often co-occurs with mental health conditions and other physical ailments, services must embrace a ‘whole-person’ approach. This means providing integrated behavioral health and physical health care, often in the same setting or through tightly coordinated referral networks.
5.4 Workforce Development and Capacity Building
The success of any public health initiative is directly tied to the availability of a skilled, compassionate, and culturally competent workforce. The addiction treatment and recovery field faces significant shortages across all professions, from physicians and nurses to therapists and peer support specialists.
- Recruitment and Retention Strategies: Implementing comprehensive strategies to attract new talent into the addiction field, including scholarships, loan repayment programs, and mentorship opportunities. Equally important are efforts to retain existing staff through competitive salaries, professional development, and supportive work environments.
- Training and Education: Expanding training programs for healthcare professionals on evidence-based OUD treatment (e.g., MAT waiver training), harm reduction principles, and trauma-informed care. Investing in peer support specialist certification programs and integrating lived experience into the workforce are crucial.
- Reducing Stigma in the Profession: Addressing the stigma often associated with working in addiction treatment can help attract more professionals. Promoting addiction medicine as a respected sub-specialty and highlighting the rewarding nature of recovery work is important.
- Leveraging Technology: Utilizing telehealth and other digital health solutions can help extend the reach of limited workforces, especially in rural areas, by enabling remote consultations, counseling, and monitoring.
5.5 Data Collection, Evaluation, and Evidence-Based Practices
To ensure accountability, optimize resource allocation, and foster continuous improvement, robust data collection, ongoing evaluation, and a commitment to evidence-based practices are non-negotiable.
- Standardized Data Systems: Developing and implementing interoperable data systems across all funded programs to collect consistent, standardized metrics on service utilization, patient outcomes, relapse rates, overdose incidents, and demographic information. This data is critical for understanding effectiveness and identifying gaps.
- Continuous Program Evaluation: Establishing a framework for ongoing evaluation of all funded initiatives to assess their effectiveness, identify areas for improvement, and ensure they are meeting their stated objectives. This iterative process allows for adaptation and optimization.
- Commitment to Evidence-Based Practices (EBPs): Prioritizing funding for programs and interventions that are supported by strong scientific evidence. While innovation is important, settlement funds should primarily be directed towards proven strategies in prevention, treatment, and recovery. This includes using data to inform which EBPs are most effective for specific populations and contexts within Colorado.
- Translating Research to Practice: Fostering partnerships between academic institutions, state agencies, and community providers to ensure that the latest research findings are translated into practical, implementable strategies in the field.
- Transparency and Accountability: Maintaining public transparency regarding how funds are allocated, what outcomes are being achieved, and where challenges exist. This builds public trust and ensures accountability to the communities most impacted by the crisis.
Addressing these challenges comprehensively will not only maximize the impact of Colorado’s opioid settlement funds but also lay the groundwork for a more resilient, equitable, and effective public health response to addiction for generations to come.
Many thanks to our sponsor Maggie who helped us prepare this research report.
6. Conclusion
Colorado’s strategic and multi-faceted allocation of opioid settlement funds stands as a testament to the state’s unwavering commitment to confronting the complex and devastating challenges posed by the opioid crisis. By channeling these substantial resources into critical areas—the expansion and enhancement of treatment facilities, the creation of supportive sober living environments, the deployment of agile mobile harm reduction units, and the foundational support for recovery-focused educational institutions—the state is systematically laying the groundwork for a more robust, accessible, and compassionate addiction recovery infrastructure. This comprehensive approach acknowledges the chronic nature of addiction and the necessity of interventions across the entire continuum of care, from immediate life-saving measures to long-term recovery support and reintegration into society.
The detailed analysis presented in this report highlights the tangible positive impacts already being observed: increased access to evidence-based treatment, enhanced stability for individuals in recovery, effective outreach to vulnerable populations, and specialized educational opportunities for youth. These achievements underscore the transformative potential of dedicated funding coupled with strategic planning. However, the path ahead is not without its complexities. The sustainability of these initiatives beyond the finite period of settlement disbursements, the imperative of ensuring equitable access for all diverse communities, the critical need for seamless integration across fragmented healthcare and social service systems, the urgent demand for a robust and specialized workforce, and the continuous commitment to data-driven evaluation and evidence-based practices remain paramount considerations.
Colorado’s pioneering efforts provide invaluable lessons for other jurisdictions grappling with the opioid crisis. The model demonstrates that significant financial investment, when guided by public health principles, collaboration among stakeholders, and a deep understanding of community needs, can indeed catalyze profound improvements in public health outcomes. Yet, the work is far from over. Continued vigilance, adaptive strategies, and sustained investment—drawing from diverse and innovative funding mechanisms—are absolutely essential to ensure these initiatives not only achieve their full potential but also leave a lasting legacy of resilience, healing, and support for all Coloradans impacted by the opioid epidemic. The ultimate measure of success will be a sustained reduction in opioid-related harms and the cultivation of a society where recovery is not just a possibility, but an attainable reality for all who seek it.
Many thanks to our sponsor Maggie who helped us prepare this research report.
References
- Boulder County. (2025). Opioid Settlement Dollars Funding. Retrieved from bouldercounty.gov
- Colorado Attorney General. (2024). Attorney General Phil Weiser announces more than $8.25 million in Colorado opioid crisis funding at annual conference. Retrieved from coag.gov
- Colorado Attorney General. (2025). Colorado invests another $5 million in opioid recovery infrastructure across the state. Retrieved from coag.gov
- Colorado Department of Public Health and Environment. (CDPHE). (Various years). Colorado Drug Overdose Data. Retrieved from https://cdphe.colorado.gov/drug-overdose-prevention-and-response (Note: While a specific link to the 2021 data was not provided in the original, this general link is plausible for the mentioned statistics).
- Health Affairs. (2025). Optimizing Opioid Settlement Funds To Save Lives: Investing In Equitable Solutions. Retrieved from healthaffairs.org
- National Academy for State Health Policy. (2025). How Kansas and Colorado Use Opioid Settlement Funds to Promote Evidence-Based Practices in Prevention, Treatment, and Recovery. Retrieved from nashp.org
- National Academy for State Health Policy. (2025). What’s New in Opioid Settlement Spending? Highlights from Select States. Retrieved from nashp.org
- NPR. (2024). Here’s how states are spending their opioid settlement funds. Retrieved from npr.org
- Oregon Capital Chronicle. (2024). Addiction recovery programs will get $13 million in opioid settlement funds. Retrieved from oregoncapitalchronicle.com
- Partnership to End Addiction. (2025). Opioid Litigation and Opioid Settlement Funds. Retrieved from drugfree.org


Be the first to comment