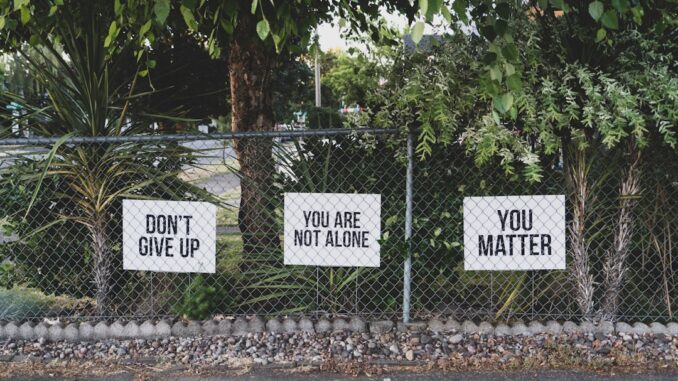
Navigating the complexities of opiate addiction, for individuals and their loved ones, can feel like an impossible climb up a sheer rock face. It’s a journey often fraught with despair, overwhelming cravings, and the heavy weight of stigma. But let me tell you, from what I’ve seen and learned, this isn’t a dead-end street. Recovery? It’s not just a hopeful whisper; it’s an absolute, tangible reality for so many. And the path there, while demanding, becomes clear when you combine the power of medication-assisted treatment (MAT), the deep insights of behavioral therapies, and the unwavering strength of a robust support system. These aren’t just buzzwords, you know? They are the fundamental pillars upon which lasting freedom from addiction is built, providing a truly holistic approach that tackles both the body’s physical dependence and the mind’s intricate patterns.
The Foundational Role of Medication-Assisted Treatment (MAT)
Think of MAT not as a crutch, but as a crucial bridge. It’s about leveraging FDA-approved medications to really soften the brutal edges of withdrawal symptoms, quell those relentless cravings, and ultimately, stabilize someone’s life so they can actually engage in the deeper work of recovery. This isn’t just about swapping one substance for another; that’s a common misconception, isn’t it? Instead, it’s a scientifically-backed approach that significantly improves outcomes. We’re talking about medications like methadone, buprenorphine, and naltrexone, each playing a distinct, incredibly effective role in treating opiate use disorder.
Methadone, for instance, is an opioid agonist. What does that mean exactly? Well, it essentially activates the same opioid receptors in the brain as illicit opioids, but it does so in a controlled, stable way. This action prevents the agonizing withdrawal symptoms that can send someone spiraling back to use, and it also blocks the euphoric effects of other opioids. For someone struggling with a severe dependence, methadone treatment, often dispensed daily from specialized clinics, provides a consistent, therapeutic dose that allows their brain chemistry to normalize. It’s a bit like giving a hyperactive engine a smooth, steady fuel supply instead of sporadic, high-octane bursts. This stability allows individuals to hold jobs, rebuild relationships, and focus on therapy without the constant physiological torment of withdrawal.
Then there’s buprenorphine, often combined with naloxone (like in Suboxone) to prevent misuse. Buprenorphine is a partial opioid agonist, meaning it only partially activates those opioid receptors. This gives it a ‘ceiling effect,’ which means that even if you take more, the opioid effects don’t significantly increase, reducing the risk of overdose. It’s also incredibly effective at reducing cravings and withdrawal symptoms. The beauty of buprenorphine-based treatments is their flexibility; they can be prescribed in an office setting by certified doctors, allowing for more integrated care within a person’s community. We’ve seen innovative forms emerge too, like Sublocade, an injectable buprenorphine that provides a month of sustained relief, and Probuphine, an implant that lasts six months. Imagine the relief of not having to think about daily medication, freeing up mental space for living. It’s transformative.
On the other hand, you have naltrexone. Now, this one’s different. It’s an opioid antagonist. Rather than activating receptors, it blocks them. Completely. If someone takes naltrexone and then tries to use an opioid, they won’t feel anything. No high, no rush. This makes it an excellent option for individuals who have already completed detoxification and are motivated to remain abstinent. The extended-release injectable form, Vivitrol, which is administered once a month, has been a game-changer for many. I remember a conversation with a colleague who once told me about a client of theirs; a young man, tired of the constant battle, who found Vivitrol to be the ‘invisible shield’ he needed. It wasn’t a magic bullet, of course, but it gave him the crucial breathing room to build new coping skills. A study published in the New England Journal of Medicine highlighted this effectiveness, showing that extended-release naltrexone injections dramatically improved recovery outcomes, with lower relapse rates and no overdose events compared to counseling alone. That’s a powerful endorsement, isn’t it?
Choosing the right MAT depends on so many individual factors, including the severity of the dependence, personal history, and even lifestyle. But the bottom line remains: MAT saves lives. It’s a cornerstone, providing the stability needed to embark on the deeper, often more challenging, psychological work of recovery.
Unpacking Behavioral Therapies: Addressing the Root Causes
While MAT does incredible work on the physical front, it’s behavioral therapies that truly dive into the intricate psychological landscape of addiction. This is where we start unpicking those deeply ingrained thought patterns, challenging problematic behaviors, and healing the underlying wounds that so often fuel substance use. It’s not always easy, but it’s absolutely essential for lasting change.
One of the most widely used and effective therapies is Cognitive-Behavioral Therapy, or CBT. This approach operates on the premise that our thoughts, feelings, and behaviors are all interconnected. If you can change your thinking, you can change your feelings and, subsequently, your actions. In the context of addiction, CBT helps individuals identify the triggers—those people, places, things, or even emotions that lead to cravings or a desire to use. Then, it equips them with practical, healthier coping mechanisms. For instance, someone might learn to recognize a pattern where stress at work leads them to think, ‘I need a way to unwind, a quick escape.’ CBT helps them challenge that thought, perhaps replacing it with ‘I need a healthy way to manage this stress,’ and then practicing alternatives like deep breathing, exercise, or calling a trusted friend. It’s about building a whole new mental toolkit for navigating life’s challenges without turning to substances. Relapse prevention strategies are a huge part of this too, teaching individuals how to anticipate high-risk situations and develop specific plans to navigate them safely.
Then there’s Motivational Interviewing, or MI. This isn’t about lecturing someone or telling them what to do. Far from it. MI is a collaborative, person-centered approach designed to strengthen an individual’s motivation for change by exploring and resolving their ambivalence. Many people struggling with addiction feel torn; they want to change, but a part of them also values the perceived benefits of substance use. MI gently guides them to articulate their own reasons for change, helping them find their internal drive. It’s incredibly empowering because the ideas for change come from within them, not from an external source. As a professional, it’s fascinating to watch someone’s eyes light up when they realize they hold the power to change, not just me, or their family, or some program.
And let’s not forget Family Therapy. Addiction doesn’t just affect the individual; it ripples through the entire family system. Family therapy brings loved ones into the recovery process, which is so crucial. It improves communication, helps repair strained relationships, and educates everyone about addiction as a disease, not a moral failing. This approach often addresses issues like co-dependency, enabling behaviors, and the emotional toll on family members. When everyone’s on the same page, working together, the support system becomes incredibly robust. I recall a family I worked with where years of addiction had shredded their trust and communication. Through family therapy, slowly, painfully sometimes, they started to hear each other again. It was a beautiful, messy process, but deeply healing.
But the therapeutic landscape is actually broader than just these. Dialectical Behavior Therapy (DBT), for example, initially developed for borderline personality disorder, is incredibly effective for addiction, particularly for those who struggle with intense emotions and impulsive behaviors. DBT focuses on four core skills: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. Learning to sit with uncomfortable feelings instead of immediately reacting, or building better ways to communicate needs, are vital for sustained recovery. And Contingency Management (CM), while sometimes misunderstood, uses positive reinforcement—like vouchers or small incentives—to encourage desired behaviors, such as negative drug tests. It might sound simple, but the immediate, tangible reward can be a powerful motivator in the early stages of recovery.
Think of these therapies as building blocks, each one adding strength and stability to the recovery foundation. They teach skills, challenge perceptions, and ultimately, empower individuals to reclaim agency over their lives. It’s a deep dive, yes, but profoundly rewarding.
Building Robust Support Systems: The Power of Community
Recovery, truly, isn’t a solitary endeavor. Trying to go it alone, well, that’s often a recipe for feeling utterly isolated and overwhelmed. The reality is, enduring recovery flourishes within a nurturing network, a strong, vibrant community that understands, supports, and holds space for the journey. This is where robust support systems come into play, weaving together a crucial safety net.
Engaging with support groups, like the widely recognized Narcotics Anonymous (NA), provides an invaluable sense of community. Here, individuals share their lived experiences, their struggles, and their triumphs in a safe, judgment-free zone. The core of NA, built on the 12 Steps, offers a structured pathway for personal growth and spiritual awakening, focusing on surrender, self-reflection, and service to others. Hearing someone say, ‘I’m Jane, and I’m an addict,’ followed by a room full of people responding, ‘Hi, Jane,’ creates an immediate connection, a palpable sense of belonging. It’s a shared understanding that transcends words, born from walking a similar, often harrowing, path.
But NA isn’t the only option. For those who prefer a different philosophy, there’s SMART Recovery, which uses science-based tools and self-empowerment principles derived from CBT and MI. Or Celebrate Recovery, a Christ-centered program. The key is finding a group where you feel comfortable and connected, where the shared experience fosters hope and accountability. It’s like finding your tribe, isn’t it? A place where you don’t have to explain yourself because everyone just gets it.
Beyond formal groups, family involvement remains critically important. Educating and involving family members can profoundly strengthen the support system. This means understanding addiction as a disease, setting healthy boundaries, avoiding enabling behaviors, and focusing on their own healing too. Sometimes, family members need their own support groups, like Nar-Anon or Al-Anon, to navigate the complexities of loving someone with an addiction. It’s a dance, really, of learning how to support without sacrificing your own well-being. It’s not always perfect, there are stumbles, but the effort to connect, to communicate, it pays dividends.
Then there are peer recovery coaches. These incredible individuals have lived experience with addiction and recovery. They’ve walked through the fire, emerged on the other side, and now dedicate themselves to guiding others. A peer coach isn’t a therapist or a sponsor; they’re a mentor, a confidant, someone who can say, ‘I know exactly how you feel, I’ve been there,’ and mean it with every fiber of their being. They offer practical guidance, encouragement, and a powerful sense of hope, demonstrating that long-term recovery is genuinely attainable. Their perspective is unique and invaluable; they’re often the first to spot when someone’s struggling, offering a hand before a setback becomes a full-blown relapse.
And let’s not overlook the broader community resources. Sober living environments, for example, provide a safe, structured, drug-free place to live while rebuilding life skills. Vocational training, educational opportunities, and assistance with housing or legal issues can also be vital components of a comprehensive support system. Recovery isn’t just about abstaining; it’s about rebuilding a whole new life, brick by painstaking brick. It’s a big undertaking, and you won’t want to do it alone.
The Holistic Horizon: Crafting a Personalized Recovery Plan
Ultimately, there’s no one-size-fits-all blueprint for overcoming opiate addiction. Just as every individual is unique, so too must be their path to recovery. The true magic happens when you weave together all these elements—MAT, behavioral therapies, and robust support systems—into a highly personalized treatment plan. This integrated, holistic approach is what significantly enhances the chances of successful, sustained recovery. We’re talking about addressing the physical dependence, certainly, but also the deep psychological patterns, and importantly, the social and environmental factors that play such a massive role.
One critical aspect often overlooked is the presence of co-occurring mental health disorders, often referred to as dual diagnosis. It’s not uncommon for someone struggling with opiate addiction to also be grappling with depression, anxiety, PTSD, or bipolar disorder. If these underlying mental health issues aren’t addressed simultaneously, recovery can feel like an endless uphill battle. A comprehensive treatment plan must integrate therapy and potentially medication for both the addiction and any co-occurring mental health conditions. Imagine trying to drive with a flat tire and then only fixing the engine; you’re not going to get far, are you?
Beyond formal treatment, lifestyle changes are incredibly powerful allies. Nutrition, for instance, plays a huge role in restoring brain chemistry and overall well-being. Regular exercise—even just a daily walk—can significantly boost mood and reduce stress. Mindfulness practices like meditation or deep breathing can help regulate emotions and build self-awareness. And let’s not forget the crucial role of adequate sleep; a well-rested mind is far better equipped to handle cravings and navigate challenges. These might seem like small pieces, but together, they create a foundation of physical and mental resilience that’s indispensable.
Long-term recovery, you see, isn’t just about stopping drug use. It’s about a complete transformation of life—learning new coping skills, building healthy relationships, finding purpose, and creating a life that is so fulfilling, so rich, that the desire for old patterns fades into the background. It’s a continuous process, a journey with its own twists and turns, highs and lows. There will be good days, and there will be incredibly tough days. Setbacks, even relapses, can happen. They’re painful, yes, but they don’t erase progress. Instead, they can become powerful learning opportunities, moments to re-evaluate and strengthen the recovery plan. It’s about getting back up, dusting yourself off, and taking the next right step. Nobody’s perfect, and this journey, perhaps more than any other, highlights our shared humanity and capacity for resilience.
Remember, recovery is not a destination you arrive at and then check off a list. It’s an ongoing journey, a process of continuous growth and self-discovery. But with the right blend of personalized strategies, professional guidance, and a loving, unwavering support network, it’s not just achievable; it’s an opportunity to build a life far richer and more meaningful than you might have ever imagined. It truly is.


Be the first to comment