Navigating the Treacherous Waters: Conquering Anxiety in Addiction Recovery
Embarking on the path to recovery from addiction, it’s not just a journey, is it? It’s often a seismic shift, a profound re-engineering of one’s entire existence. And let’s be honest, it demands immense courage, a kind of quiet heroism really. But alongside the Herculean task of overcoming substance dependence, many individuals encounter a persistent, often unwelcome companion: anxiety. This dual struggle, addiction and its ever-present anxious shadow, can feel profoundly overwhelming, like trying to climb a mountain during a thunderstorm. Yet, with the right strategic tools, a good support system, and a fair bit of grit, it’s absolutely possible to navigate both successfully, to find your footing and even, eventually, some peace.
The Intricate Dance: Unpacking the Addiction-Anxiety Connection
Now, it’s really not uncommon for anxiety to co-occur with addiction, you know. In fact, it’s probably more common than not. Think about it: a significant number of people initially turn to substances as a desperate means to self-medicate, to quell the relentless chatter of an anxious mind, or to dull the sharp edges of panic. Alcohol, opiates, benzodiazepines — they can all, at first anyway, offer a fleeting sense of calm, a deceptive pause from the storm. But here’s the insidious trap, and it’s a deep one: this approach almost invariably exacerbates the problem, weaving a vicious cycle that’s extraordinarily difficult to unravel. That initial ‘fix’ merely kicks the can down the road, leading to a rebound anxiety that’s often far worse than the original state. You drink to calm nerves, then wake up with withdrawal-induced anxiety, so you drink again. It’s a self-perpetuating nightmare.
Recognizing this profound connection, understanding that these aren’t isolated battles but deeply intertwined struggles, that’s truly the first critical step toward effective management and, ultimately, sustainable recovery. We’re talking about ‘dual diagnosis’ or ‘co-occurring disorders’ here, a complex interplay where mental health issues like anxiety and substance use disorders feed off each other, complicating treatment if not addressed concurrently. When the brain has adapted to a substance, its natural neurotransmitter balance goes haywire. Remove the substance, and you’re left with a nervous system screaming for equilibrium, often manifesting as acute anxiety, restlessness, and insomnia. It’s like trying to untangle a ball of yarn that’s been knotted for years; you can’t just pull on one thread and expect it all to come loose. You need an integrated approach, something that tackles both the addiction and the anxiety simultaneously.
Anchoring in the Present: The Power of Mindfulness Meditation
Mindfulness meditation, once considered a fringe practice, has deservedly gained immense traction, hasn’t it? For its remarkable ability to significantly reduce anxiety and genuinely enhance emotional well-being, it’s become a cornerstone of many recovery programs. This ancient practice, at its heart, involves simply focusing on the present moment, observing thoughts, feelings, and sensations without judgment. And for those in recovery, grappling with cravings, regrets, and fears about the future, it’s particularly beneficial. It helps to calm those racing thoughts, to quiet the internal critic, and to nurture a much-needed sense of inner peace, even if it’s just for a few moments at first.
To begin practicing mindfulness, you don’t need a meditation cushion or an incense stick, honestly. Just find a quiet space, maybe a comfortable chair in a sunny corner of your apartment, where you can sit undisturbed. Close your eyes gently and begin to take slow, deep breaths. The key here is to really pay attention to each breath – feel the cool air as it enters your nostrils, notice your chest expanding, and then feel the warmth as the breath leaves your body. When thoughts inevitably intrude – and they will, don’t worry, that’s just what minds do – simply acknowledge them without judgment. Don’t engage with them, don’t follow them down a rabbit hole. Just notice them, maybe even label them as ‘thinking,’ and then gently, patiently guide your focus back to your breathing. It’s like training a puppy; it wanders off, you gently bring it back. There’s no failure in this practice, only repeated opportunities to return to the present.
Over time, by consistently incorporating even ten or fifteen minutes of mindfulness meditation into your daily routine, you can really begin to change your brain, literally. It helps you manage anxiety by fostering a deeper sense of calm, reducing the reactivity that often leads to substance cravings, and building a stronger, more resilient emotional core. You learn to observe urges without immediately acting on them, to create a vital space between stimulus and response. I remember one fellow, David, he used to say he felt like his brain was a pinball machine, constantly lighting up with anxious thoughts. After a few months of daily mindfulness, he confided, ‘It’s like the machine’s still there, but someone finally unplugged it. I can just watch the lights now, they don’t drag me into the game.’ It’s a powerful shift, believe me.
A Natural Uplift: Physical Activity as a Stress Reliever
Engaging in regular physical activity isn’t just about looking good, you know, though that’s a nice bonus. It offers a profoundly natural and incredibly effective way to combat anxiety. When you move your body, whether it’s a brisk walk around the block, a heart-pumping jog, a flowing yoga session, or even just letting loose in a dance class in your living room, your body releases endorphins. These aren’t just ‘feel-good’ chemicals; they’re your body’s natural mood lifters, powerful stress reducers, and they can significantly diminish feelings of anxiety. Beyond the neurochemical rush, simply moving your body not only distracts from obsessive, anxious thoughts but also promotes overall well-being, improves sleep, and boosts self-esteem. It’s a multi-faceted win.
Consider Sarah, the 32-year-old I mentioned earlier, navigating the early days of recovery. She really struggled with persistent anxiety, those nagging intrusive thoughts, and a constant battle with cravings. Her days often felt like wading through treacle. But she decided to try running, just short distances at first, pushing herself a little further each time. Initially, it was tough, a real grind, but as she incorporated running into her daily routine, something remarkable started to happen. She noticed a significant, almost palpable, reduction in her anxiety levels. The physical exertion provided a healthy outlet for her pent-up energy and emotional tension, and the rhythmic motion of her feet on the pavement became a form of moving meditation. Moreover, she found a newfound sense of accomplishment, a quiet confidence that radiated into other areas of her life. ‘Each mile,’ she once told me, ‘felt like I was running away from the old me and towards something better. And I swear, the cravings got quieter, almost like they were out of breath trying to keep up.’ What’s not to love about that?
And it’s not just running, by the way. Anything that gets your heart rate up and your muscles working can be beneficial. Yoga, for example, combines physical postures with breath work and mindfulness, offering a holistic approach to stress reduction. Swimming can be incredibly meditative, the rhythmic strokes washing away worries. Even weightlifting can provide a sense of empowerment and control. The key is finding an activity you genuinely enjoy, something you can stick with, because consistency, as with all these strategies, is paramount.
Reshaping Thought Patterns: The Practicality of Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy, or CBT, is a powerhouse, honestly, a widely used and incredibly effective technique in both anxiety management and substance abuse recovery. Its core focus is on identifying and then actively altering the negative, often distorted, thought patterns that consistently contribute to anxiety and fuel addictive behaviors. It operates on the premise that our thoughts, feelings, and behaviors are all interconnected. If you can change the way you think, you can change the way you feel and behave. By directly challenging these entrenched, unhelpful thoughts, CBT empowers individuals to develop healthier, more adaptive coping strategies. It’s not about positive thinking as much as it’s about realistic and helpful thinking.
The practical, structured nature of CBT makes it particularly effective. It’s not just talk therapy; it’s hands-on, equipping individuals with concrete tools to recognize triggers, manage stress effectively, and significantly reduce the risk of relapse. Therapists often guide clients through specific exercises, like thought records where you document an activating event, your resulting thoughts, feelings, and then evaluate the evidence for and against your thoughts. You learn to spot cognitive distortions, those sneaky ways our minds trick us into believing unhelpful things: catastrophizing, black-and-white thinking, overgeneralization. For instance, if you have a slight setback in recovery, an anxious thought might be, ‘I’m a complete failure, I’ll never get this right.’ CBT helps you challenge that: ‘Is it really a complete failure? What evidence do I have? Is it possible this is just a stumble, and I can learn from it?’
This structured approach not only addresses immediate anxiety symptoms – helping you breathe through a panic attack or calm a racing heart – but also builds profound resilience for long-term recovery. It teaches you how to become your own therapist, in a way, giving you the mental tools to navigate future challenges. It’s a comprehensive solution for those grappling with co-occurring disorders, offering a roadmap for sustainable change. Many clients I’ve seen initially resist the ‘homework’ aspect of CBT, the worksheets, the thought tracking. But almost without exception, they come back surprised by how much insight they’ve gained and how much calmer they feel when they actively engage with the process. It’s a game-changer, really.
Strength in Numbers: Building a Robust Support Network
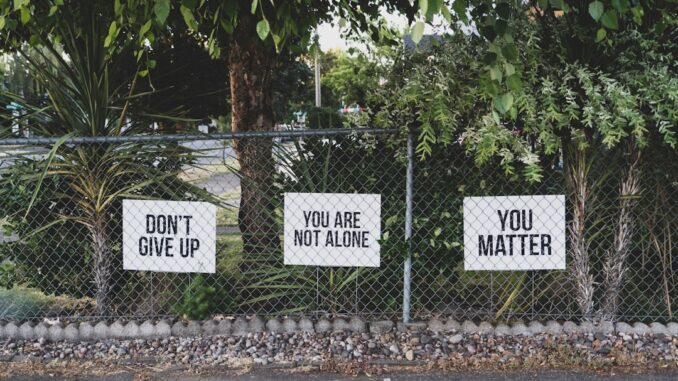
Let me tell you, recovery doesn’t have to be a solitary journey, and frankly, it shouldn’t be. Trying to go it alone is like trying to lift a car by yourself; you might move it an inch, but you’ll burn out quickly. Building and diligently maintaining a strong support network is, in my opinion, absolutely essential. Engaging with individuals who share similar experiences, who understand the unique struggles and challenges of recovery, provides an unparalleled sense of belonging. This connection is truly crucial for navigating the bewildering complexities of recovery, those emotional rollercoasters, and sudden urges. These connections aren’t just for emotional comfort; they offer practical advice, shared wisdom gleaned from hard-won battles, and a powerful sense of ‘you are not alone.’
Support groups like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) are classic examples, and for good reason. They facilitate structured group meetings, offering a safe, confidential space to express struggles, celebrate achievements, and learn from others. These settings, grounded in shared experience and mutual respect, encourage accountability, something many in active addiction lose sight of. They also provide tangible tools and a framework, like the 12 Steps, to help manage anxiety and prevent relapse. But the landscape of support is much broader now. Alumni programs from treatment centers offer ongoing connections. Family therapy can help heal strained relationships and build a supportive home environment. And for those unable to attend in-person meetings, perhaps due to location or social anxiety, online forums and virtual meetings have become invaluable resources, extending the reach of community support globally. Peer networks, mentors, sponsors – they all contribute to creating a dense fabric of community, making the recovery process feel less isolating, less overwhelming. It’s powerful, genuinely, to sit in a room and hear someone else voice exactly what you’ve been feeling, to realize you’re not the only one fighting this fight. The sense of camaraderie is palpable, a lifeline for so many.
The Bedrock of Well-being: Cultivating a Balanced Lifestyle
Prioritizing deliberate lifestyle adjustments can profoundly alleviate anxiety, setting a stable foundation for recovery. It’s not just about what you stop doing, but crucially, about what you start doing to build a life worth living. This isn’t just fluffy wellness advice; these are non-negotiable components of mental and physical health. Developing a regular exercise routine, as we discussed, practicing mindfulness or meditation daily, and perhaps most critically, ensuring adequate, restorative sleep – these all contribute significantly to stress reduction and overall emotional regulation. These practices don’t just feel good; they actively help manage withdrawal symptoms and mitigate cravings by stabilizing mood and energy levels.
But let’s dive deeper. Sleep hygiene, for instance, is often overlooked but profoundly impactful. Chronic sleep deprivation can mimic anxiety symptoms, making everything feel worse. Establishing a consistent sleep schedule – going to bed and waking up at the same time every day, even on weekends – trains your body’s internal clock. Creating a relaxing bedtime routine, making your bedroom dark, cool, and quiet, and avoiding screens for an hour before bed can work wonders. Remember, sleep isn’t a luxury; it’s a biological necessity, especially in recovery.
Nutrition also plays an incredibly vital role. Your brain needs fuel, good fuel. Eating balanced meals, rich in whole foods, lean proteins, complex carbohydrates, and healthy fats, helps stabilize mood fluctuations and provides sustained energy. Conversely, a diet high in sugar, processed foods, and excessive caffeine can actually exacerbate anxiety and contribute to energy crashes that trigger cravings. Think gut-brain axis: an unhealthy gut microbiome has been linked to increased anxiety and depression. So, incorporating probiotic-rich foods like yogurt or fermented vegetables, and plenty of fiber, can literally improve your mood. I’ve seen people cut out sugary drinks and feel a noticeable drop in their baseline anxiety levels within weeks.
Then there’s stress management beyond exercise and mindfulness. This includes learning to say ‘no,’ setting healthy boundaries in relationships, and not over-committing. It also means incorporating joy and purpose. What hobbies did you enjoy before addiction took over? Revisit them. Learn something new. Volunteer your time. Finding meaning outside of substance use, a sense of contribution or personal growth, fills the void that addiction once occupied. Journaling, for example, can be an incredibly constructive avenue for processing complex feelings, allowing individuals to confront and challenge specific anxieties, phobias, and fears that inevitably arise during recovery. It provides a safe space for self-reflection, a chance to get those swirling thoughts out of your head and onto paper, where they often lose some of their power. You might discover patterns in your anxiety, triggers you hadn’t noticed before, simply by writing it all down.
The Personalized Toolkit: Developing Tailored Coping Strategies
Effective coping skills are not just helpful; they’re truly essential for relapse prevention, especially when anxiety is a constant, unwelcome guest. Recovery is never a one-size-fits-all endeavor, and neither should your coping toolkit be. It’s imperative you work closely with your treatment team – your therapist, counselor, or sponsor – to develop a personalized arsenal of techniques that resonate with your unique needs and challenges. What works for one person might not resonate with another, and that’s perfectly okay. The goal is to build a diversified portfolio of strategies you can deploy when anxiety flares up or cravings hit.
This personalized toolkit might include:
- Grounding techniques for panic moments: When anxiety threatens to overwhelm you, pulling you out of the present, grounding techniques can be invaluable. The ‘5-4-3-2-1’ method is a popular one: identify 5 things you can see, 4 things you can feel, 3 things you can hear, 2 things you can smell, and 1 thing you can taste. This redirects your focus to your immediate environment, away from the internal storm. Other techniques include holding an ice cube, splashing cold water on your face, or firmly pressing your feet into the ground. These sensory inputs can interrupt the panic cycle.
- Regular stress-reduction practices: Beyond daily exercise and mindfulness, consider deep breathing exercises like diaphragmatic breathing, progressive muscle relaxation (tensing and releasing different muscle groups), or even a warm bath with essential oils. Consistency here is key; these aren’t just for crisis moments but for daily preventative maintenance.
- Healthy boundaries in relationships: This is a big one. Anxiety often stems from a feeling of lack of control or being overwhelmed by external demands. Learning to assert yourself, to say ‘no’ without guilt, and to protect your energy is a crucial anxiety management skill. It also helps in avoiding situations or people that might trigger urges or heighten stress.
- Sleep hygiene routines: As we touched upon, prioritizing consistent, quality sleep is non-negotiable. This involves creating a conducive sleep environment, winding down effectively before bed, and avoiding stimulants like caffeine and nicotine, especially in the afternoon and evening.
- Journaling to track anxiety triggers: Keeping a journal allows you to become a detective of your own mind. Note down when your anxiety spikes, what you were doing, who you were with, and what thoughts were running through your mind. Over time, patterns will emerge, allowing you to proactively avoid or prepare for high-risk situations.
- Relapse prevention planning: This isn’t just about avoiding substances; it’s about having a concrete plan for how you will cope with difficult emotions or unexpected life events that could lead to relapse. What are your personal triggers? Who will you call? What specific strategies will you employ? Having these answers ready dramatically increases your chances of navigating challenges successfully.
By carefully tailoring these coping strategies to your unique needs, your triggers, and your preferences, you can better manage anxiety, reduce the risk of relapse, and truly support your recovery journey. It’s an ongoing process, a continuous refinement, but each step builds on the last.
Knowing When to Raise the Flag: Seeking Additional Professional Help
Look, while all these strategies are powerful and incredibly important, it’s also vitally important to recognize when anxiety crosses a line, when it demands additional, specialized professional support. There’s no shame in it, none at all. Think of it like this: if you had a broken leg, you wouldn’t hesitate to see a doctor, would you? Mental health is no different.
Warning signs that might indicate a need for more intensive intervention include:
- Anxiety that severely impacts daily functioning: This means it’s not just a passing worry; it’s preventing you from going to work, engaging with loved ones, leaving the house, or maintaining personal hygiene. When anxiety dictates your life, it’s time to seek help.
- Panic attacks that don’t respond to your current coping strategies: These aren’t just moments of intense fear; they’re often characterized by sudden, overwhelming physical symptoms like a racing heart, shortness of breath, dizziness, sweating, and a terrifying sense of impending doom. If your grounding techniques aren’t cutting it, you need more support.
- Thoughts of self-harm or suicide: This is a critical red flag, a serious emergency. If you’re experiencing these thoughts, even fleetingly, it’s absolutely crucial to reach out immediately. Call a helpline, tell a trusted friend or family member, or go to an emergency room. Your life is precious, and support is available to help you through these dark moments.
- Increasing urges to return to substance use specifically to cope with anxiety: This is a classic sign that your current strategies are insufficient. If the pull back to old habits is getting stronger because anxiety feels unbearable, you need to bring in the pros.
If you’re experiencing any of these symptoms, please understand that a wealth of resources are available to provide appropriate, specialized support. This might involve a psychiatrist who can assess for medication options (which can be life-changing for severe anxiety), a specialized trauma therapist if past experiences are fueling your anxiety, or a dual diagnosis treatment program that explicitly addresses both your addiction and your mental health concurrently. It’s about finding the right level of care, the right experts, who can provide the tools you need when your own just aren’t enough. Remember, reaching out isn’t a sign of weakness; it’s a testament to your strength and your unwavering commitment to your own recovery. You wouldn’t try to build a house without proper tools and guidance, would you? Your mental well-being deserves no less consideration.
Incorporating these robust strategies into your personalized recovery plan can truly help you manage anxiety effectively, paving the way for a healthier, more fulfilling, and dare I say, happier life. It’s a marathon, not a sprint, this journey of recovery. There will be good days and bad days, breakthroughs and setbacks. But remember this: you’re absolutely not alone in this journey, and support is truly available, ready to guide you, every single step of the way. Believe in your ability to heal, to grow, and to thrive. You’ve already taken the bravest step, haven’t you?


Be the first to comment